RESOURCES
Review Articles
Book Chapters
- Encyclopedia of Endocrine Disease (2018); Thyroid Gland: Anatomy & Physiology
OBJECTIVES & QUESTIONS
Anatomy & Macrascopic Structure
What is the macrascopic structure of the thyroid gland?
- H-shaped, highly vascular gland:
- Has two lateral lobes (left and right) approx. 4cm long and 2cm wide
- Isthmus bridging them approx. 3cm wide and 2cm high
- 50% of people have a pyramidal lobe arising from the superior isthmus directed upwards or to the left
- Located in the neck between C5 and T1 vertebrae:
- Anteriorly: platysma, sternothyroid, and sternohyoid muscles (strap muscles)
- Posteriorly: deep cervical fascia, condensing to form the Berry’s ligament which anchors it to the trachea at the first and second tracheal rings
- Laterally: overlaps the carotid sheath and its components
- Parathyroid glands located within the posterior surface of the lateral lobes:
- Usually four (two superior and two inferior)
- About the size of a grain of rice
Microscopic Structure
What is the microscopic structure of the thyroid gland?
- Functional unit of the thyroid is the follicle:
- Outer sphere of cuboidal epithelial cells (thyrocytes) and thin basement membrane:
- Site of thyroglobulin production
- Filled with a protein-rich core called colloid:
- Made up of thyroglobulin, a large glycoprotein
- Serves as the main storage of thyroid hormones
- Outer sphere of cuboidal epithelial cells (thyrocytes) and thin basement membrane:
- C-cells are dispersed between follicles to produce calcitonin
Overview & Functions
Which hormones are produced by the thyroid gland?
Hormone
Function
Thyroxine (T4) - carries 4 iodine atoms)
Regulation of metabolism and growth
Triiodothyronine (T3) - carries 3 iodine atoms)
Regulation of metabolism and growth
Reverse-triiodothyronine (r-T3) - formed by peripheral conversion of T3
Metabolically inactive
Calcitonin
Regulation of calcium and phosphate levels (lowers serum levels through deposition in bone and renal excretion)
What are the effects of thyroid hormones (T3 & T4)?
Effects on Metabolism
- Increase basal metabolic rate of most tissues (Long duration of action):
- Increased heat production
- Increases cardiac metabolic rate:
- Ionotropic / chronotropic effect
- Increased lipolysis & gluconeogenesis
Effect on Beta Receptors
- Increases number and sensitivity of B adrenoceptors
- Sensitises catecholamines
- Sensitises effects of insulin
- Increase in heart rate (HR) and myocardial contractility leading to an increase in cardiac output
Effect on Growth and Development
- Increases Growth hormone
- Vital in growth and development of nervous system:
- Neuronal myelination
- Nerve axon growth
What is the difference between T3 & T4?
T3
- Active form of thyroid hormone - 3x more potent than T4
- 20% of T3 secreted directly from the thyroid
- 80% converted peripherally from T4
T4
- Often referred to as the prohormone due to low biological coactivity
- Approximately 90% is converted in peripheral tissues to more active T3 form - principally in the liver and kidneys
- Can also be converted to metabolically inactive reverse T3 (rT3)
- Fasting increases the ratio of rT3:T3.
Synthesis & Transport
How are thyroid hormones synthesised, stored and released?
Can be considered in 4 steps:
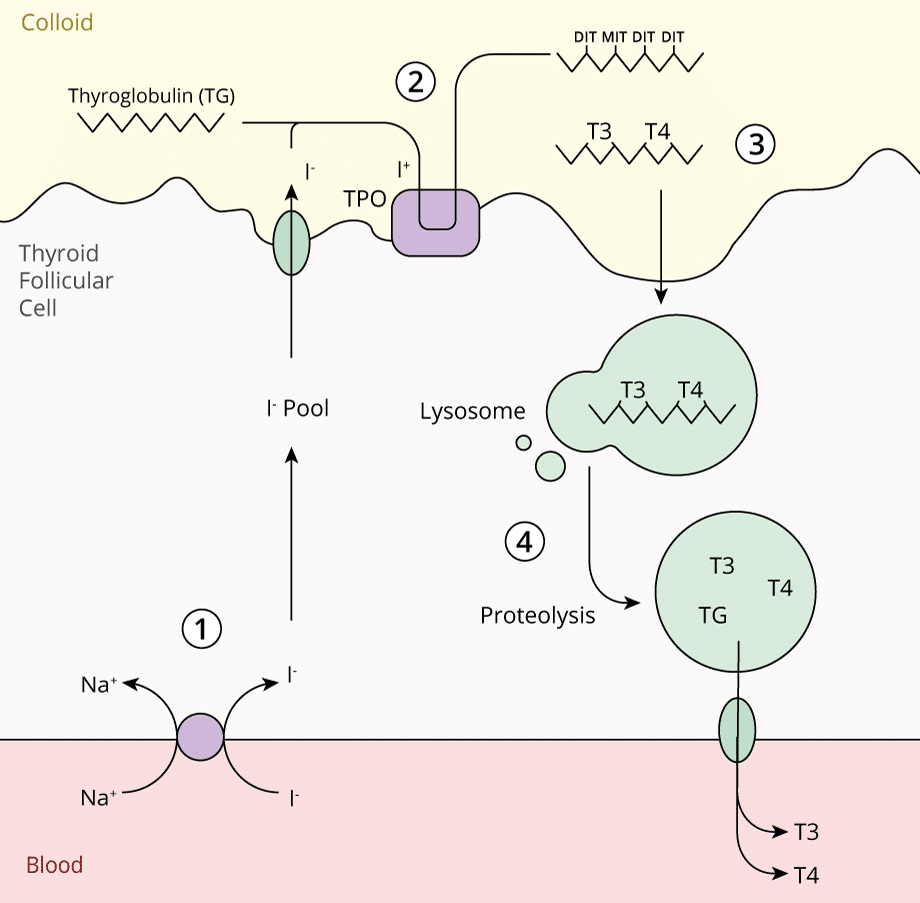
1. Iodide Trapping
- Iodine obtained in diet from dairy, grains and meat (150mg/day required)
- Reduced to the inorganic form iodide (I-)
- Actively taken up by thyroid follicular cells, stimulated by TSH:
- Transported against a concentration gradient by Na+/I- Symporter (NIS)
2. Iodide Oxidation & Organification
- Moves apically in the cell where is oxidised to iodine (I+)
- Requires the membrane bound enzyme thyroperoxidase
- I+ covalently binds to tyrosine residues on thyroglobulin in the colloid
- May be iodinated at one or two positions forming:
- Monoiodotyrosine (MIT)
- Diiodotyrosine (DIT)
3. Storage in Colloid with Thyroglobulin
- Tyrosine residues couple to form precursors of thryroid hormones:
- MIT & DIT couple to form T3
- DIT & DIT couple to from T4
- T3 & T4 remain attached to the thyroglobulin molecule for storage in colloid
4. Secretion of Thyroid Hormones
- When stimulated by TSH, thyroglobulin is internalised into the thyrocyte membrane via endocytosis
- Lysosomal endopeptidase cleaves the thyroglobulin releasing T3 and T4
- Thyroid hormones are released into the cytoplasm and diffuse into the bloodstream through the basement membrane
How are thyroid hormones transported in the blood?
- <1% transported freely in plasma unbound to plasma proteins:
- Forms the active portion of the hormone
- Mostly transported by non-covalent binding to plasma proteins:
- Thyroid binding globulin (TBG) – 75%
- Transthyretin – 20%
- Albumin – 5%
- TBG has 10x the affinity for T4 than T3:
- Therefore T3 is more readily available and is removed from the circulation
Action & Receptors
How do thyroid hormones (T3 & T4) exert their action?
- Thyroid hormones exert their actions via intranuclear receptors
- Enter cells via membrane transporter proteins
- Bind to intranuclear receptors causing activation and conformation changes
- Allows binding of the complex to specific “thyroid responsive” sections of DNA, leading to DNA transcription and gene expression
Which receptors do thyroid hormones act on?
There are to major subtypes of thyroid receptors (TR-α and TR-β) each with their own isoforms:
TR-α1
- Widely expressed
- Particularly high expression in cardiac and skeletal muscle
TR-α2
- Widely expressed
- Unable to bind hormone
- Function unclear
TR-β1
- Brain, liver and kidney
TR-β2
- Hypothalamus and pituitary
Regulation
How are thyroid hormones regulated?
- Thyroid hormone production is regulated by a series of negative feedback loops
- Thyroid stimulating hormone (TSH) is an important regulator:
- Peptide hormone produced in the anterior pituitary gland
- Stimulates the production and release of thyroid hormones
- TSH production is stimulated by:
- TRH production
- Low serum levels of thyroid hormones
- TSH production is inhibited by:
- High serum levels of thyroid hormones (negative feedback loop)
- High serum levels of TSH (ultra-short negative feedback loop)
- Thyrotropin-releasing hormone (TRH) is another important regulator:
- Peptide hormone produce in the hypothalamus
- Stimulates the production and release of TSH
- TRH production is stimulated by:
- Low serum levels of thyroid hormones
- Hypothermia (particularly in infants)
- TRH production is inhibited by:
- High serum levels of thyroid hormones (negative feedback loop)
- Stress