OBJECTIVES & QUESTIONS
Thyroid Hormones
Which thyroid hormones are measured routinely and what is their clinical utility?
Hormone
Normal Level
Description
Thyroid Stimulating Hormone (TSH)
0.27 - 4.2 mU/L
- A measure of plasma TSH which is produced by the pituitary gland in response to thyrotropin-releasing hormone and stimulates production and secretion of thyroid hormones
- Usually considered the best initial test in the diagnosis of thyroid disease:
- Elevated levels can suggest hypothyroidism
- Decreased levels suggest hyperthyroidism
- Serial measurements can be used to manage thyroid hormone therapy
Free Thyroxine (FT4)
12 - 22 pmol/L
- A measure of the metabolically active quantity of thyroxine, which circulates unbound to serum proteins
- Used to determine thyroid over or underactivity in the setting of an abnormal TSH;
- Elevated levels can confirm thyrotoxicosis
- Decreased levels can confirm hypothyroidism
Total Thyroxine (T4)
5 to 12 μg/dL
- A measure of total T4 in the plasma, including both and unbound forms
- Abnormal levels despite normal thyroid function can be caused by conditions which alter levels of thyroid binding globulin:
- Drugs or illness can increase the thyroid biding proteins available to carry T4 and increase total levels despite a constant absolute concentration of free "active hormone"
- An example is pregnancy or hyper oestrogenic states which increase levels of TBG and thus increase levels of total T4
Total Triiodothyronine (T3)
3.1 - 6.8 pmol/L.
- A measure of the metabolically active quantity of T3:
- The major source of T3 comes from peripheral conversion of T4
- Can be used to confirm hyperthyroidism:
- Hyperthyroidism usually associated with greater increase in T3 than T4
- Small proportion of patients with hyperthyroidism have a normal T4 but an elevated T3 (so called "T3 toxicosis")
- Conversely many patients with hypothyroidism have normal T3 levels
- T3 levels are often decreased in clinically euthyroid patients with non-thyroidal illness (so called "sick-euthyroid syndrome"
- Difficulty in interpreting abnormal results makes it a poor initial screening test
What is the initial screening test of choice for diagnosis of thyroid dysfunction?
- TSH traditionally recommended as first-line screening as levels often change markedly in response to small variations in thyroid hormones
- Screening with TSH values alone can lead to misdiagnosis:
- TSH values may be normal despite significant hypothalamic-pituitary dysfunction meaning conditions are missed
- Abnormal levels do not differentiate between clinical and sub-clinical disease
- Most laboratories use combined TSH and fT4 levels as an initial screening test
Additional Tests
Which autoantibodies are useful in the diagnosis of thyroid disease?
Antibody
Primary Association
TGAb
Thyroglobulin antibody
Thyroglobulin antibody
Hashimoto's thyroiditis
TPOAb
Thyroid peroxidase antibody
Thyroid peroxidase antibody
Hashimoto's thyroiditis
TSAb
TSH Receptor Stimulating Antibody
TSH Receptor Stimulating Antibody
Grave's disease
TBAb
TSH Receptor Blocking Antibody
TSH Receptor Blocking Antibody
Atrophic Thyroiditis
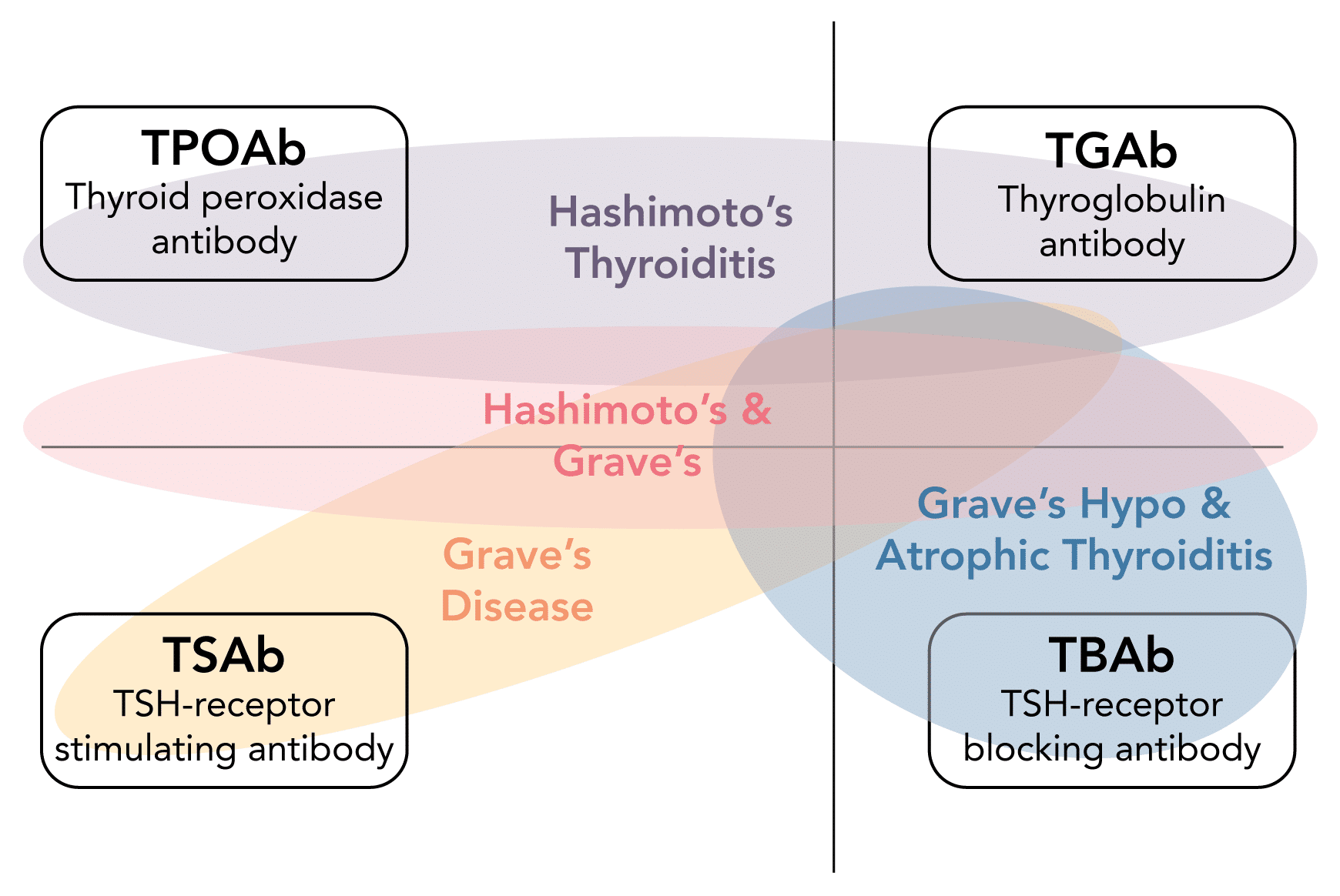
Which diseases are the thyroid autoantibodies associated with?
- Autoimmune thyroid disease represents a spectrum of disease
- Each antibody can be associated with a range of clinical conditions
TFT Patterns
What are the common hormone abnormalities seen in thyroid disease?
TSH
Free T4
Free T3
Condition
Normal
Normal
Normal
None
↓
↑
↑
Hyperthyroidism
↓
Normal
Normal
Subclinical Hyperthyroidism
↓
Normal
↑
T3 Toxicosis
↓
↑
Normal
Thyroiditis
T4 Ingestion
T4 Ingestion
↓
↓
↓
Secondary hypothyroidism
Sick Euthyroid syndrome
Sick Euthyroid syndrome
↑
Normal
Normal
Subclinical hypothyroidism
Recovery from Sick Euthyroid syndrome
Recovery from Sick Euthyroid syndrome
↑
↓
↓
Primary hypothyroidism
↑
↑
↑
Secondary Hyperthyroidism
What is meant by subclinical disease?
- Thyroid dysfunction is reflected by abnormal TSH levels
- Reference ranges for thyroid hormones are wide and changes significant enough to render a patient hypo- or hyperthyroid may still be numerically within normal limits (sub-clinical disease)
Which TFT patterns can be seen in non-thyroidal illness?
- Three patterns of change in thyroid hormone levels have been described in non-thyroidal illness:
NTI Pattern
TSH
Free T4
Free T4
Free T4
Explanation
Low T3 Syndrome
(Sick euthyroid syndrome)
(Sick euthyroid syndrome)
Normal
↓
N or ↑
Normal
Likely due to reduced peripheral conversion of T4 to T3 by the 5′ deiodinase enzyme
Low T4 Syndrome
Normal
↓
N or ↑
↓
In some patients, serum T4 levels also fall (the low T4 syndrome). Low T4 levels in patients with severe nonthyroidal illness have been associated with increased mortality. TBG levels may be reduced in such patients, and an inhibitor of T4 binding to TBG has been described in the serum of such patients
High T4 Syndrome
Normal
↓
N or ↑
↑
High T4 nonthyroidal illness syndrome probably involves one or more induced abnormalities in the disposal pathways of T4
Which abnormal TFT patterns can be seen with commonly used drugs?
Drug
TSH
Free T4
Explanation
Amidarone
Transient
↑
↑
Transient
↑
↑
- Common during the first few months due to inhibition of DIO preventing peripheral conversion of T4 to T3
Amidarone
↓
↑
- Thyrotoxicosis can occur due to:
- Large iodine load in drug precipitating thyroid autonomy
- Destructive drug induced thyroiditis
Amidarone
↑
↓
- Hypothyroidism due to failure to escape from Wolff-Chaikoff effect
Lithium
↑
↓
- Overt or subclinical hypothyroidism
Lithium
↓
↑
- Drug induced thyroiditis
Tyrosine Kinase Inhibitors
↑
↓
- Primary hypothyroidism due to direct toxic effect
Tyrosine Kinase Inhibitors
↓
↑
- Prodromal thyrotoxic phase may be seen