RESOURCES
OBJECTIVES & QUESTIONS
Structure & Function
What are intra-aortic balloon pumps?
- A circulatory assist device that can provide temporary support to a failing heart
- Acts through a number of mechanisms which improve coronary perfusion, augment diastolic pressure and result in increased cardiac output
What are the components of an intra-aortic balloon pump?
Catheter
- Catheters between 7.5-8 Fr
- Inner lumen monitors systemic arterial pressure and connects to pressure transducer
- Outer lumen supplies gas to balloon
Balloon
- Made of polyurethane
- Inflation volumes of 30-50cc
- 150-270mm in length
- Size determined by patient height
Console
Contains a number of elements:
- Gas cylinder (usually helium)
- A valve unit allowing delivery of the gas
- A monitor system for ECG and arterial blood pressures
- Control unit to process timing of balloon inflation and deflation
What is the function of the balloon?
- Function of the balloon is to provide “counterpulsation” – describes the cycles of:
- Inflation in diastole
- Deflation in early systole
- Inflates at onset of diastole:
- Caused by delivery of a set volume of gas through pneumatic systems
- Fills 80-90% of thoracic aortic diameter causing ‘volume displacement’ of blood both proximally and distally
- Increases diastolic pressure, improving coronary and systolic perfusion
- Deflates at onset of systole, prior to ejection:
- Due to rapid removal of gas following a predetermined time interval
- Leads to an effective vacuum effect, improving blood flow down aorta
- Pressure in the balloon is measured and displayed as a waveform
Which gas is used to inflate the balloon?
Both helium and carbon dioxide have been used:
Helium
- Most commonly used driving gas in modern practice
- Low density facilitating faster filling and emptying times
- Low blood solubility with potential for embolisation
CO2
- Greater blood solubility lowering risks of embolization
- Higher density limits rapid inflation and deflatio
Physiological Effects
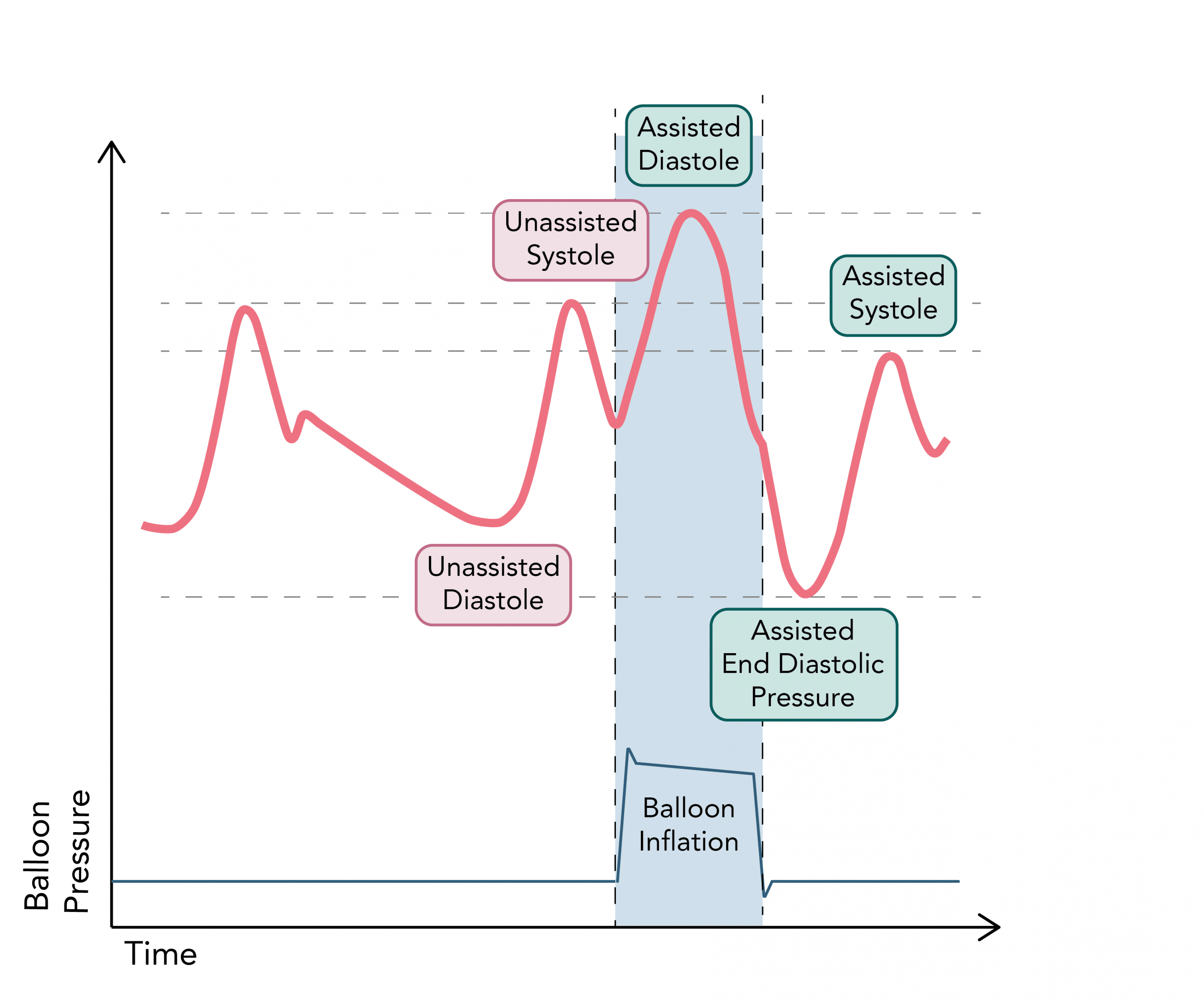
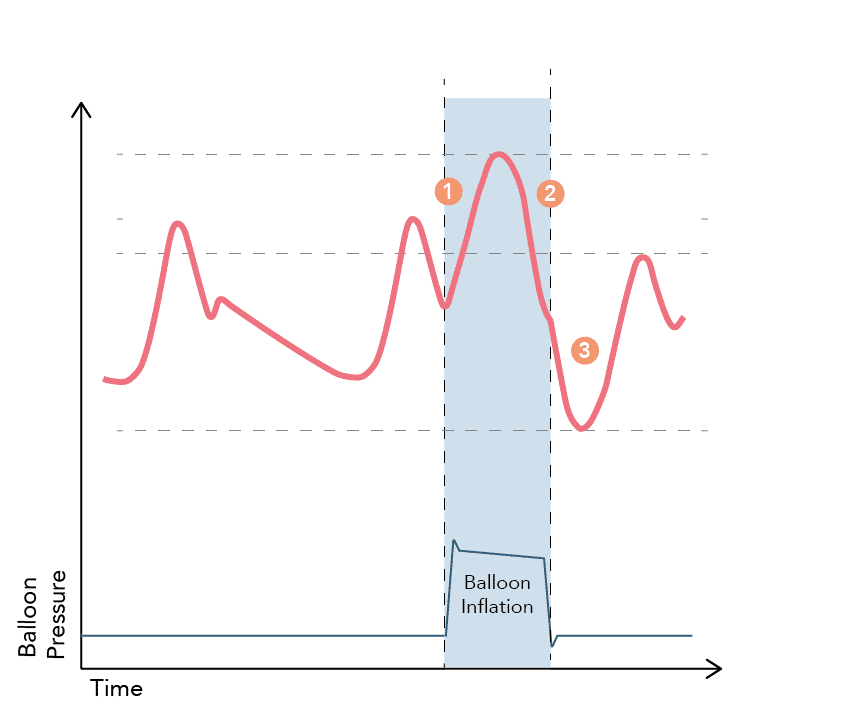
What does a normal Intra-aortic balloon pump (IABP) pressure tracing look like and why?
1. Balloon inflation occurs at the onset of diastole, synchronously with aortic valve closure and the appearance of the dichroitic notch . The displacement of blood results in a rapid rise in aortic pressure (known as assisted / augmented diastole) leading to “active” coronary artery perfusion.
2. The pressure falls as the elastic energy in the tissues of the aorta is converted into kinetic energy of the aortic blood flow
3. Balloon deflation occurs at the beginning of systole during isovolumetric contraction, causing an effective reduction in afterload. This causes the end-diastolic and systolic aortic pressures to be reduced (assisted end-diastole and systole)
2. The pressure falls as the elastic energy in the tissues of the aorta is converted into kinetic energy of the aortic blood flow
3. Balloon deflation occurs at the beginning of systole during isovolumetric contraction, causing an effective reduction in afterload. This causes the end-diastolic and systolic aortic pressures to be reduced (assisted end-diastole and systole)
What are the beneficial physiological effects of IABPs?
Effect of Inflation
- Volume displacement results in increased diastolic pressure (30%):
- Increases coronary perfusion pressure and flow
- Increases myocardial oxygen delivery
- Higher mean pressure increases renal and systemic perfusion
Effects of Deflation
- Decreased afterload, and thus systolic pressure (10%), immediately following deflation:
- Vacuum like effect promotes forward flow and increases stroke volume
- Decreases end diastolic volume and ventricular wall stress
- Reduces myocardial oxygen demand
Overall Effects
- Improved ratio of myocardial oxygen supply to myocardial oxygen demand
- Improved myocardial performance and increased cardiac output (up to 20%)
Timing & Triggers
What are the ideal timings for balloon inflation & deflation?
Inflation
Onset of diastole just after the closure of the aortic valve
Deflation
Onset of systole during isovolumetric contraction
What can be used to trigger balloon inflation and deflation?
Trigger
Timings
Use & Limitations
ECG
Inflation: Middle of the T wave
Deflation: Peak of the R wave
Deflation: Peak of the R wave
Requires good ECG trace. May not be suitable if arrythmia present
Arterial Pressure Waveform
Inflation: At the dicrotic notch
Deflation: Just before the systolic upstroke
Deflation: Just before the systolic upstroke
Requires the balloon pump to accurately sense ventricular systole and diastole
Asynchronous / Internal
Timings based upon pacing spikes depending upon mode
Requires patient to be 100% paced. Should not be used for on demand pacing
Pacing Device
Asynchronous augmentation based on a set rate (40-120/min)
Rarely used except in cases of cardiac arrest
Indications & Contraindications
What are the indications for using IABPs?
- In general, IABP should only be used for conditions that are
- Reversible or as a bridge to definitive treatment
- Acute, life-threatening and unresponsive to conventional treatment
- Evidence is limited for its use but it remains a regularly utilised therapy
Conditions Benefiting from Diastolic Coronary Perfusion
- Cardiogenic shock while waiting for PCI
- Intractable ischemia awaiting revascularization
- Pulmonary oedema in spite of maximal medical management
- Cardiogenic shock complicating MI (controversial indication)
Conditions Benefiting from Reduced Afterload
- Weaning from cardiac bypass
- As a bridge to cardiac transplant
- Significant pathology with haemodynamic compromise awaiting repair:
- Severe aortic stenosis
- Mitral regurgitation
- Other mechanical complications of MI
- Ventricular septal defect
- Complex paediatric congenital cardiac disease
- Cardiogenic shock complicating MI (controversial indication)
Prophylactic Indications
- High risk CABG patients (pre-op)
- High-risk PCI patients (pre-op)
What is the evidence for the use of intra-aortic balloon pump in cardiogenic shock secondary to MI?
- A recent large RCT failed to show benefit of routine use in cardiogenic shock secondary to MI
- Lack of evidence to support its use has led to removal from guidelines as a recommendation as therapy for this indication
- However it continues to be used as a rescue measure based on expert consensus
Intervention
Population
Conclusion
- IABP insertion and counter pulsation vs. medical therapy alone
- 600 patients across 37 centres
- Inclusion criteria: MI (STEMI or NSTEMI), planned revascularisation and cardiogenic shock
- No significant difference in all cause 30-day mortality (39.7% vs. 41.3%, P=0.69)
- No significant difference in any secondary outcomes
What are the contraindications to the use of an IABP?
Absolute
- Patient refusal
- Irreversible or end-stage cardiac disease
- Aortic regurgitation (anything more than mild)
- Aortic dissection
- Aortic stents
- Severe aortic atheromatous disease
- Severe peripheral vascular disease
Relative
- Severe neurological deficit
- Compromising tachyarrhythmias
- Abdominal aortic aneurysm
- Sepsis
- Arterial tortuosity
- Contraindications to anticoagulation including coagulopathy and HIT
- LVOT obstruction
Complications
What are the complications of using an IABP?
Vascular
- False aneurysm
- Aortic dissection
- Haematoma formation
- Vascular injury at time of insertion
- Peripheral thrombotic embolization
- Limb ischaemia & compartment syndrome
- Tamponade
Position Related
- Upper limb ischemia (too proximal)
- Spinal cord, renal and visceral ischaemia (too distal)
- Cerebral ischaemia
- Limb compartment syndrome
Balloon Related
- Balloon rupture and helium embolus
- Immobility - balloon becomes lodged
- Thrombocytopenia and haemolytic anaemia
Other
- Infection (Insertion site or disseminated)
Insertion & Management
How is an IABP Inserted?
- Balloon catheters are inserted percutaneously through an introducer sheath using the Seldinger technique
- The most common site for insertion is the femoral artery
- Alternative sites include subclavian, brachial or iliac arteries
- Fluoroscopic guidance is usually used to guide positioning
- Once in situ, the IABP is usually not uncomfortable
What size IABP are used?
- A number of IABPs are available with different balloon volumes and lengths
- Augmentation is maximised when stroke volume is equal to balloon volume
- The correct size is primarily selected based upon the height of the patient
- Sizes vary between manufacturers but an example of commonly used sizing is shown below:
Height
Balloon Volume
Balloon Length
Balloon Diameter
<152 cm
25cc
180 mm
13 mm
152-162 cm
34cc
219 mm
14.7 mm
162-183 cm
40cc
260 mm
15 mm
>162 cm
50cc
270 mm
18 mm
Where should an IABP be positioned?
- Balloon catheters are inserted percutaneously through an introducer sheath using the Seldinger technique
- The most common site for insertion is the femoral artery
- Alternative sites include subclavian, brachial or iliac arteries
- Fluoroscopic guidance is usually used to guide positioning
- Once in situ, the IABP is usually not uncomfortable
How should a patient with an IABP be managed?
- Should be managed in an appropriate area by staff familiar with IABP management
- To minimize the risk of proximal catheter migration:
- Should be log rolled
- End of the bed should not be elevated to more than 30 degrees
- Regular assessments should include:
Patient
- Vital signs and the need for augmentation
- Blood pressure from IABP console even if another arterial line is in situ
- Hourly assessment of limb perfusion:
- Colour, capillary return, sensation and presence of pulses by palpation or Doppler studies
- Presence of limb ischaemia should prompt consideration of removal of the device and sheath and urgent vascular surgery review
- Assessment insertion site for oozing, bleeding, swelling and signs of infection.
Investigations
- Regularly assessment of:
- Haemoglobin (risk of bleeding or haemolysis)
- Platelet count (risk of thrombocytopenia)
- Renal function (risk of acute kidney injury secondary to distal migration of IABP catheter)
- Coagulation parameters
Balloon Pump
- Ensure consistent triggering and correct timing
Troubleshooting & Timing
What are some common problems that may result in failure of the IABP to augment?
Failure to augment may be due to:
- Inappropriate timing of inflation or deflation of the balloon
- Inappropriate balloon size
- Balloon misplaced too proximal or too distal
- Balloon inadvertently placed in a false passage
What are the problems that can occur with inappropriate timing of an IABP?
Timing
Physiological Effect
Waveform Features
Waveform
Early Inflation
- Potential premature closure of aortic valve
- Reduction in cardiac output
- Increased LVEDV and LVEDP
- Increased myocardial oxygen consumption.
- Balloon inflates before dicrotic notch
- Diastolic augmentation encroaches onto systole
- May be difficult to distinguish between two peaks
Late inflation
- Inflation of the IAB markedly after closure of the aortic valve
- Reduction in duration of diastolic augmentation Suboptimal coronary artery perfusion
- Balloon inflates after the dicrotic notch
- Absence of sharp ‘V’ in the trace with reduced height of the diastolic augmentation peak
Early Deflation
- Reduction in duration of diastolic augmentation
- Suboptimal coronary perfusion and potential for retrograde flow
- Suboptimal afterload reduction
- Increased myocardial oxygen consumption
- Sharp decrease after diastolic augmentation
Late Deflation
- Deflation of the IAB after the onset of systole
- Increased myocardial oxygen consumption
- Prolonged isovolumetric contraction phase
- Increased afterload
- Reduction in cardiac output
- Diastolic augmentation may appear widened
- Assisted aortic end-diastolic pressure increased and may equal unassisted pressure
- Rate of systolic pressure rise is prolonged
Weaning & Removal
When should be a patient be weaned from an IABP?
- Institutions may have their own criteria that should be achieved prior to weaning
- In general, the following should be present:
- Adequate cardiac output:
- Cardiac Index (CI) >2.2 L/min/m2
- Drop in CI <20% when attempting to wean IABP
- Minimal inotropic support
- Absence of angina
- Urine output >30mL/hr
- Heart rate <100 beats/min
- No signs of systemic hypoperfusion
- Adequate cardiac output:
How can a patient be weaned from an IABP?
- There are two primary options for weaning from IABP
Reducing Augmentation Ratio
- Ratio of augmented to non-augmented beats can be reduced from ratios of 1:1 to 1:2 to 1:3
- The timing of augmentation reduction is usually every 1-6 hours depending upon the individual clinical picture
- If a ratio of 1:3 is tolerated for 6 hours then the device should be removed
Reducing Augmentation Volume
- Volume of balloon augmentation can be decreased by 10ml until a lower limit of 20ml is reached
- Again, the timing of volume reduction is usually every 1-6 hours depending upon the individual clinical picture
- If an augmentation volume of 20ml is tolerated for 6 hours then the device should be removed
- The risk of thrombus formation increases as the augmentation ratio or volume is decreased
- The balloon pump must not be left in situ once switched off as this is associated with a high chance of thrombus formation on the balloon and distal embolization
- Systemic anticoagulation should be corrected before removal of the catheter