RESOURCES
Guidelines
Documents
Review Articles
- Cheung, Resp Care (2014); Tracheostomy: Epidemiology, Indications, Timing, Technique, and Outcomes
- Batuwitage, CEACCP (2014); Percutaneous Tracheostomy
- Ghattas, Journal of Thoracic Disease (2021); State of the art: percutaneous tracheostomy in the intensive care unit
- Lages, Sociedade Brasileira de Anestesiologia (2018); Ultrasound guided airway access
OBJECTIVES & QUESTIONS
Indications & Timing
What are the indications for a tracheostomy?
Overcome Upper Airway Obstruction (Actual or Potential)
- Tumour
- Bilateral recurrent laryngeal paresis
- Oral / facial trauma
- Infection in oral cavity, pharynx or larynx
- Burns
- Following certain head and neck surgery
Facilitate Airway Protection and Secretion Management
- Laryngeal incompetence due to critical illness, polyneuropathy, or bulbar dysfunction
- Neurological disease
- Traumatic brain injury
Facilitate Weaning from Mechanical Ventilation
- Any reversible condition requiring ventilatory support
Provide Lifelong Ventilation
- High C-spine injury
What are the advantages of a tracheostomy?
- Reduction in laryngeal and vocal cord trauma
- Prolonged intubation associated with injury such as pressure necrosis and mucosal abrasions
- Reduced sedation requirement (better tolerated than ETT)
- Facilitation of gradual weaning from mechanical ventilation:
- Reduced work of breathing
- Reduced resistance and dead space
- Improved oral hygiene
- Allows rehabilitation:
- Improved mobility, speaking, oral intake
- Improved patient communication (written or spoken)
- Improved patient comfort
- Reduced LOS in ICU
- Reduced nursing care required
Is emergency tracheostomy the surgical procedure of choice in patients with apneoa and acute upper airway obstruction when intubation fails?
- Cricothyroidotomy is the procedure of choice
- Provides greatest likelihood of successful airway placement
- Has superficial location with easily identifiable landmarks
- Complications of tracheotomy increase fivefold when used in an emergency situation
Is there any evidence to suggest early tracheostomy is superior to late tracheostomy to aid weaning from ventilation?
- No high-quality studies have definitively answered the question of whether routine, early tracheostomy improves clinical outcomes:
- Studies are difficult to design
- Doctors are poor at predicting which patients may undergo successful extubation within the next few days, thereby avoiding unnecessary tracheostomy
- Accumulated evidence and expert opinion suggest early tracheostomy does not improve survival or even shorten hospital stay
- The largest trial to explore the question is the TRACMAN trial:
Population
Intervention
Conclusion
- Intubated and ventilated patients expected to require at least seven further days of ventilation
- Excluded those with potential indications for early tracheostomy (airway obstruction, neurological illness, TBI)
- Early (within four days of admission) vs. late (on/after day 10) tracheostomy
- Primary outcome 30-day mortality
- No difference in mortality at any point over the two-year follow-up
Early group: - Non-significant trend towards shorter duration of mechanical ventilation
- Significantly fewer days of sedation administration
Late group: - Only 43% of the patients in the late group went on to receive a tracheostomy (many not intubated)
- 6.3% complication rate for the tracheostomies that were performed
- Eight RCTs with a total of 1,977 participants
- Early tracheostomy (two to 10 days after intubation) vs. late tracheostomy (> 10 days after intubation) for critically ill adult patients
- Results from seven RCTs (n = 1903) showed lower mortality rates in the early as compared with the late tracheostomy group (risk ratio (RR) 0.83, P value 0.03)
- However due to low quality evidence review concluded results "no more than suggestive of the superiority of early over late tracheostomy"
When should tracheostomies be performed during an admission?
- Timing of tracheostomy should be decided on a case-by-case basis
- Balance between the risks of an invasive and potentially unnecessary procedure with risks that of prolonged endotracheal intubation and sedation
- Should be considered when a need for prolonged ventilation becomes apparent
- Any decisions should involve the patient and the multidisciplinary team:
- Significant lifestyle considerations and burdens for both the patient and their family should be discussed
- All reasonable efforts should be explored to establish patients’ wishes
- Given lack of clear evidence guiding timing of insertion some clinicians advocate waiting at least two weeks until reaching a decision
- Some clear early indications such as airway obstruction, neurological illness, TBI)
- Most patients can undergo spontaneous breathing trial before the decision for tracheostomy
- 2014 NCEPOD report highlighted a significant proportion of patients undergo procedure without an attempt at primary extubation
How should consent be gained for tracheostomy?
- Procedure in the critically ill should almost always be planned:
- Benefits and burdens weighed up by the MDT over a period of days
- Allows ample time to explain the procedure to the patient and relatives
- Consent is considered mandatory:
- Majority of cases will use a consent form 4 for patients that lack capacity
- Where possible, attempts should be made to utilise communication aids and support to determine patient capacity and facilitate consent
Contraindications
What are the contraindications to tracheostomy insertion?
Absolute Contraindications
- Patient Refusal
- Unstable fractures of the cervical spine
- Severe local infection of the anterior neck
- Uncontrollable coagulopathy
Relative Contraindications
- Lack of need:
- Unlikely to survive >48 hours
- Unlikely to require >2 weeks ventilation
- Controlled local infection
- Coagulopathy:
- PT or APTT >1.5
- Platelets <50
- High PEEP (>10) or FiO2 (>0.6) requirements
- Difficult anatomy (contraindication to percutaneous tracheostomy, surgical tracheostomy advised):
- Abnormal or prominent vasculature at insertion site
- Morbid obesity
- Short thick neck
- Reduced neck extension
- Excessive goiter
- Tracheal deviation
- Previous radiotherapy
- Proximity to extensive burns or surgical wounds
- Elevated intracranial pressure
- Haemodynamic instability
Complications
What are the complications of tracheostomy insertion?
Immediate (During Insertion)
- Arrest and Death (1/600)
- Haemorrhage (minor or severe) - 4.8%
- Misplacement (pre-tracheal tissues or to main bronchus)
- Hypoxia
- Injury to local structures:
- Pneumothorax and surgical emphysema
- Oesophageal perforation
- Vascular injury
- Thyroid injury
- Posterior tracheal wall injury
- Laryngeal nerve damage
- Tracheal ring fracture
- Air embolism
- Equipment issues:
- Incorrect tube / size
- Equipment malfunction
Delayed (Post Insertion)
- Tube blockage with secretions (may be sudden or gradual)
- Tube migration to pre-tracheal space
- Accidental decannulation
- Infection:
- Stoma site
- Bronchial tree
- VAP
- Erosion related:
- Tracheal ulceration or necrosis
- Tracheo-oesophageal fistula formation
- Tracheo-innominate fistula
Late (Post Decannulation)
- Tracheal injury / dysfunction:
- Tracheal stenosis at the cuff site
- Tracheomalacia
- Vocal cord dysfunction
- Persistent sinus at the tracheostomy site
- Granulomata of the trachea
- Tracheo-innominate fistula
- Psychological impact related to stoma
Techniques & Advantages
What are the different techniques for a surgical airway?
Surgical Tracheostomy
- An open surgical procedure that allows insertion of a tracheostomy tube into the trachea between cartilaginous rings.
Percutaneous Dilatational Tracheostomy
- Refers to various procedures that have in common either a modified Seldinger technique for placing a modified tracheostomy tube or a forceps technique to cannulate and dilate tracheal tissue between cartilaginous rings
- Used for over 90% of ICU tracheostomies with over two-thirds of all tracheostomy procedures are now performed by intensivists in ICUs rather than by surgeons
Cricothyroidotomy
- Technique for placement of an airway into the trachea through the cricothyroid space
- Can be performed as a surgical procedure through an incision, as a percutaneous procedure by a Seldinger technique, or as a needle cricothyroidotomy for emergency airway access.
Mini Tracheostomy
- Allows percutaneous placement of a 7F cannula through the tracheal rings to allow suctioning for patients with difficulty clearing airway secretions
What are the advantages and disadvantages of surgical or percutaneous tracheostomies?
Percutaneous
Surgical
Advantages
- Relatively quick in experienced hands
- Avoids need for transfer of unstable patients
- Does not require involvement of surgeons
- Cheaper
- Smaller scar
- Tighter stoma that decreases stomal bleeding and provides better fit
- Can be performed when percutaneous contraindicated:
- Short or thick neck, obese
- Coagulopathy
- Unstable spine
- Previous neck / thyroid surgery
- Abnormal vessels
- Resources available to control bleeding
- Potentially easier management in event of early tube dislodgment or tube exchange:
- Stoma stitched open
- May have stay sutures to elevate the trachea
Disadvantages
- Suboptimal conditions for management of bleeding, especially if major vessel injured
- Blind techniques can be incorrectly positioned
- Tracheal ring fracture can occur
- Late tracheal stenosis (as per surgical tracheostomy)
- Lack of surgical dissection can increase risk of vascular or thyroid injury
- Potentially more difficult management in event of early tube dislodgment or tube exchange:
- Tissues will tend to ‘spring’ closed when tube removed in first 7–10 days
- Requires operating theatre leading to delays in insertion
- Requires patient transfer
- More expensive
Procedure (Ciagla Technique)
How do you perform a percutaneous tracheostomy?
- ICS / FFICM or Local Safety Checklist
- Intravenous anaesthesia, muscle relaxant and vasopressors
- Local anaesthetic with adrenaline
- Syringe and needle
- Sterile gloves and gown
- Protective face shield or goggles
- 2% chlorhexidine / isopropyl alcohol cleaning swabs
- Sterile procedure pack:
- Drape with window
- Gauze swabs
- Percutaneous tracheostomy set:
- Appropriately sized tracheostomy tube and spare one size smaller
- Obturator
- Needle /cannula and syringe
- Guidewire
- Scalpel
- Dilators
- Sterile saline
- Lubricating gel
- Suture (if using)
- Tube ties or device to secure
- Fibreoptic laryngoscope/bronchoscope
- Catheter mount to accept scope
- Airway equipment:
- Emergency airway trolley
- Direct +/- video laryngoscope
- I-gel or LMA
- Yankauer sucker
- Spare endotracheal tube
- Document assent and complete appropriate consent form
- Arrange a time during daytime hours
- Gather information about the patient:
- Review recent blood results and drug chart
- Review recent chest imaging
- Determine the optimal depth of ETT and recent ventilatory requirements
- Stop enteral feed and ensure NG tube aspirated
- Consider ultrasound of the neck as part of risk assessment
- Ensure skilled assistant present and assign roles
- Prepare IV access, fluids and emergency drugs
- Ensure appropriate sedation and muscle relaxation:
- Consider use of BIS to guide deep sedation
- Ensure full monitoring including EtCO2 (turned to face the operator)
- Set the ventilator:
- Pre-oxygenate with FiO2 of 1.0
- Mild hyperventilation often used with volume control ventilation
- Position the patient:
- Use a head ring
- Neck extended using pillow or bag of fluids under the shoulder blades
- Sitting up 30 degrees reduces venous distension and bleeding risk
- Complete safety checklist
- Ensure full asepsis –
- Gown/gloves/mask.
- Use of a face visor is advisable
- Prepare the site with chlorhexidine skin preparation
- Infiltrate local anaesthetic:
- Often performed prior to fully prepping the patient to allow full effect
- Use up to 20ml of 0.1% xylocaine with adrenaline
- Initially infiltrate just under skin, then a little in subcutaneous tissue allowing the skin to blanch
- Position the ETT under direct vision with laryngoscope:
- Withdraw until top of cuff just visible above the cords
- If difficult view use the bronchoscope
- Alternative is to use LMA
- Position bronchoscope to directly visualise intended insertion site within the trachea
- Insert the cannula under bronchoscopic vision
- Ideally between the second and third tracheal rings
- Aim for the midline but accept 11-1 o’clock for first puncture
- Insert the needle at 90 ° to the skin holding the trachea stable
- Aspirate continuously (with a syringe containing 2 ml of saline) until the trachea is entered and air is aspirated
- Remove the needle from within the cannula
- Insert the guide wire
- Remove the cannula
- Check the position of the wire with a bronchoscope
- Make a vertical incision:
- Approximately 10-15 mm), through the skin in the midline
- Perform initial dilatation:
- Use the short, narrow, stiff initial dilator
- Ensure the wire moves freely within the dilator at all times to avoid kinking of the wire
- Keep the dilator vertical initially, then adjust caudally
- Perform further dilatation
- Ensure the long white tube is used as it stiffens the wire and prevents kinking
- Push the tapered “rhino” dilator and the white tube firmly and smoothly together over the guidewire into the trachea, in a caudal direction
- Stop pushing when the skin is aligned with a black marker
- Insert the tracheostomy:
- Remove the tapered dilator, leaving the wire and white tube in situ
- Place the tracheostomy tube onto the loading obturator and slide both onto the wire and white tube
- Using a smooth firm action, push the tube into the trachea
- Remove the guidewire, white tube and the loading obturator
- Check the position:
- Consider using the bronchoscope to check down the tracheostomy prior to ventilation
- Using careful hand ventilation, check for rise and fall of the chest and the presence of end-tidal CO2
- Secure in place
- Perform a chest x-ray :
- Confirms position of tracheostomy
- Reveals complications such as pneumothorax
- Ensure full documentation
- Ensure bedhead sign and tracheostomy box placed with patient
Airway & Ventilatory Management
How is the airway managed during percutaneous tracheostomy insertion?
- Should be managed by a team member trained and competent to do so
- Equipment should be available for repeat intubation
- End-tidal CO2 is mandatory for the procedure
- Position the ETT under direct vision with laryngoscope:
- Withdraw until the top of cuff just visible above the cords
- Video laryngoscopy can make manipulations of the ETT easier
- If difficult use of a fibreoptic bronchoscope may be beneficial
- An alternative technique is to remove the ETT and use an LMA
- Fibreoptic bronchoscope is then used:
- Ensure correct initial placement of the introducer needle in the midline and between second and third tracheal rings
- Passed through the tracheal tube and the anatomy of the airway visualised
- Can be used to monitor dilation and confirm placement
How should the ventilator be set during percutaneous tracheostomy?
- The ventilator should be set appropriately prior to commencing the procedure
- Ensure 100% oxygen given throughout
- Consider using a volume-controlled mode and a 1:1 I:E ratio
Applied Anatomy & Landmarks
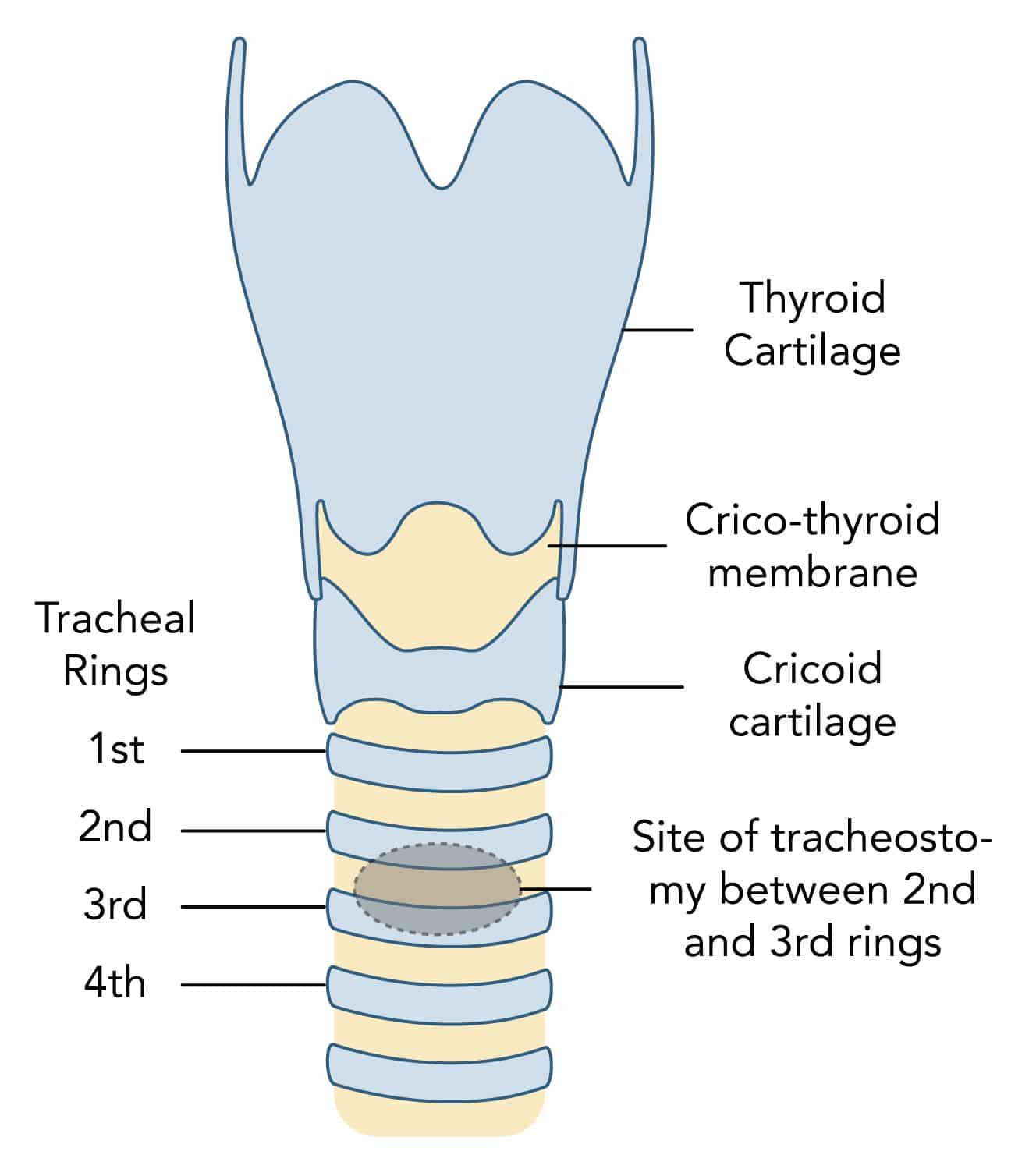
What is the preferred site of insertion for percutaneous tracheostomy and why?
- Preferred site of tracheostomy is between the 2nd and 3rd tracheal rings in the midline
- Tracheostomy above this site:
- Can lead to damage to the cricoid cartilage and first tracheal ring
- Results in increased risk of subglottic stenosis which is difficult to treat
- Tracheostomy below this site:
- Can lead to damage to the thyroid and great vessels at the root of the neck
- Results in increased risk of significant bleeding
What is the structure and course of the trachea?
- Tube of cartilage with a membranous lining continuous with the larynx
- Composed of 16–20 C-shaped cartilaginous rings
- Trachealis muscle completes the posterior wall
- Around 10-12 cm in length
- Extends down from cricoid at C6
- Terminates at carina at T5-
- Moves anteriorly to posteriorly from the cricoid distally
- Enters the chest behind the sternal notch
Which structures are in close relationship to the trachea?
Anterior Relations
- Skin and fascia
- Isthmus of thyroid
- Sternothyroid and sternohyoid muscles
- Manurbrium sternum
- Thymus gland
Lateral Relations
- Lobes of thyroid
- Carotid sheath
- Lungs and pleura
- Arch of aorta, brachiocephalic and subclavian arteries
Posterior Relations
- Oesophagus
- Recurrent laryngeal nerve
Which vessels are at risk of damage during tracheostomy?
- Anterior jugular veins:
- Run vertically close to the midline
- Thyroid ima artery :
- Ima is ‘lowest’ in Latin
- Anatomical variant in 3–10% of the population
- More common British Asian populations
- Arises mainly from the brachiocephalic trunk and ascends along the front of the trachea
- Inferior thyroid veins
- Other vessels more lateral: internal jugular vein, carotid artery, external jugular vein
What is the relationship of the thyroid to the trachea?
- Lobes lie laterally to the trachea and extend to the 6th tracheal rings
- Isthmus crosses the midline in the region of the 2-4th tracheal rings
- Pyramidal lobe, an anatomical variant, may extend superiorly from the isthmus to the cricoid
Which palpable surface landmarks in the anterior neck are useful when determining the correct site for a percutaneous tracheostomy?
Tube Selection
What is the ideal size of a tracheostomy tube for a patient?
- No ideal size for all patients and varies according to patient and clinical situation
- The best approximation is a tube with an outer diameter two thirds the inner calibre of the patients trachea
- Smaller tracheal tubes:
- May decrease the risk of tracheal stenosis given as smaller incision required
- Present issues with suctioning, ventilation and bronchoscopy
- May require higher cuff inflation pressures and potential damage to mucosa
- Larger tracheal tubes:
- Require wide stomas
- Prevent adequate cuff inflation to cushion against the rigid tube
Which factors may influence the type of tube inserted?
Secretion Management
- Tubes with sub-glottic suction port useful in patient with
- May be part of standard VAP intervention bundle
Abnormal Airway Anatomy
- Standard tubes may be unsuitable in abnormal anatomy
- Obese patients may require tube with extended proximal length (adjustable flange)
- Patients with fixed flexion deformity may not accommodate tubes with a fixed angulation
Airway Pathology
- Pathology such as tracheomalacia or granuloma formation may necessitate the use of a tracheostomy tube that has a longer distal length
Weaning and Vocalisation
- Patient who are being 'weaned' may benefit from tubes that are a smaller size than initially inserted or are uncuffed
- Allows greater gas flow and increased ease of vocalisation and laryngeal rehabilitation
Clinical Support
- For patients on less respiratory support where the risks of cleaning an inner tube are reduced, a double lumen tracheostomy tube with an inner cannula is recommended to reduce the risk of obstruction
Use of Ultrasound
What are the advantages of using ultrasound prior to a percutaneous tracheostomy?
- Determine appropriate size
- Assess appropriate site of insertion:
- Determine level of tracheal cartilages to avoid puncture above 1st ring
- Determine midline
- Determine depth to trachea
- Assess for possible abnormal anatomy:
- Presence of thyroid tissue
- Large thyroid or anterior jugular vessels in the midline
- Early recognition of pneumothorax