RESOURCES
Review Articles
OBJECTIVES & QUESTIONS
Overview & Components
What are the components of a typical tracheostomy tube?
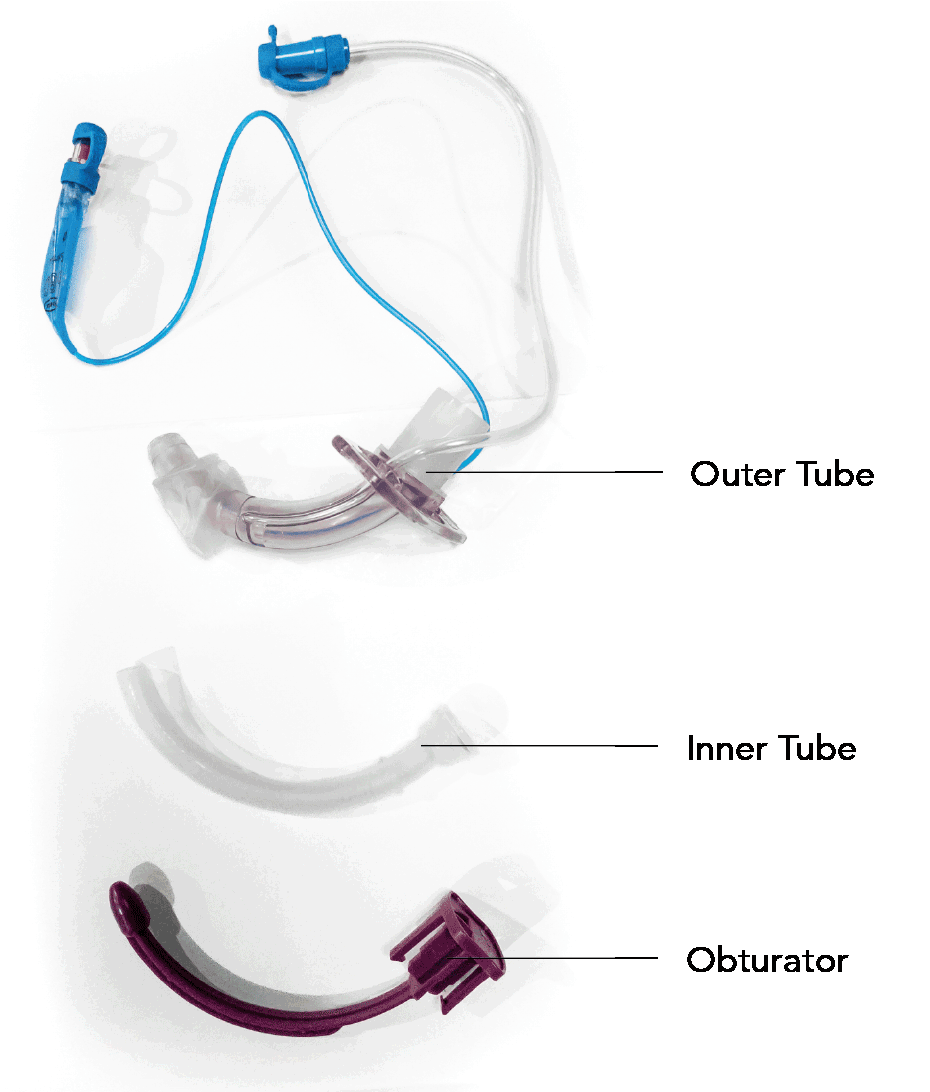
- Typically made up of three parts:
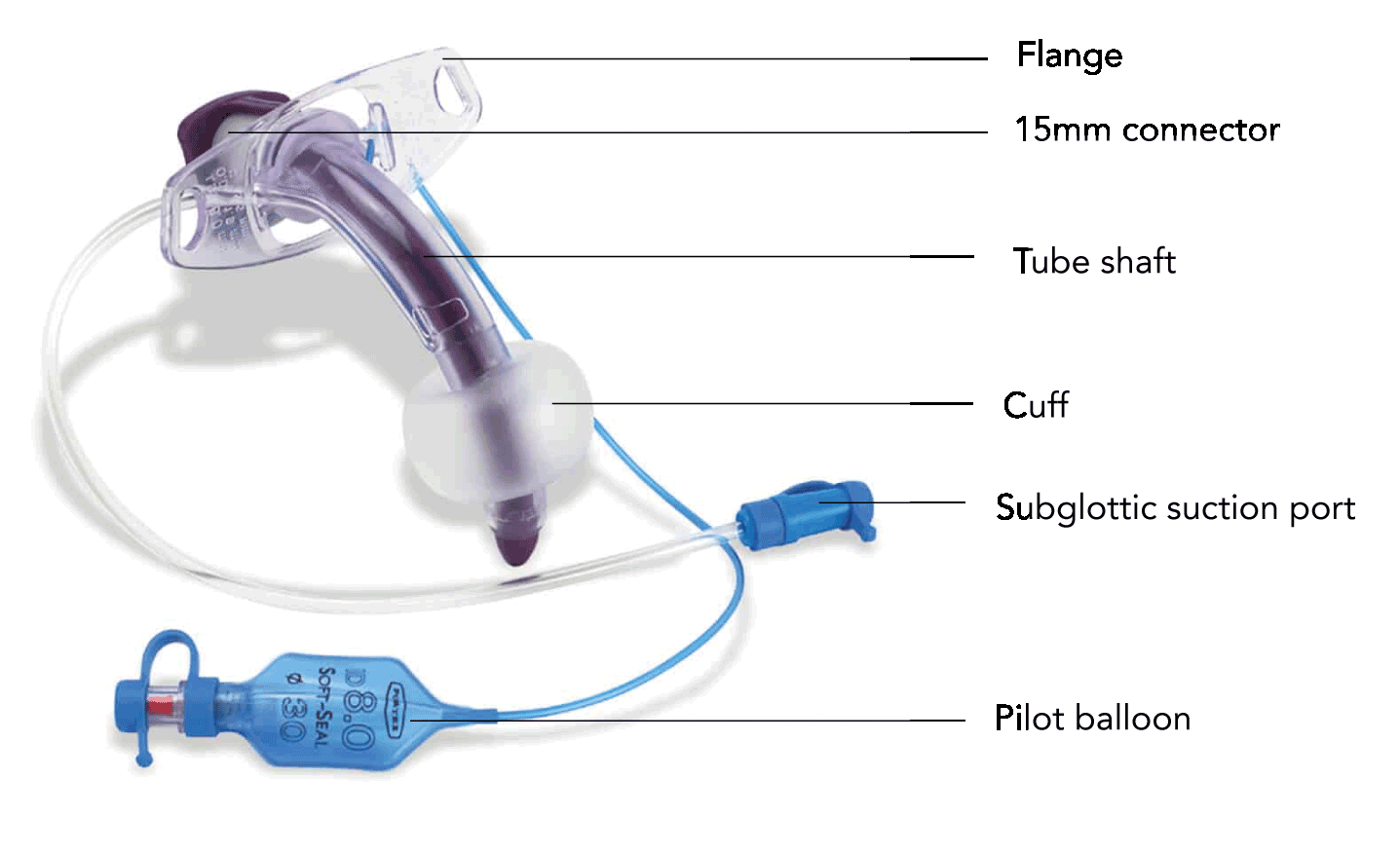
- A curved plastic tube with a proximal flange that is sutured or tied in position on the neck
- Has a proximal 15 mm connection for a breathing system (some designs require inner tube to be places to connect to a standard 15mm circuit)
- A simple plastic sleeve that slides inside the outer tube
- May easily be removed to allow cleaning or if plugged with secretions
- Paediatric tubes are often of a single-cannula design (without an inner tube)
- A plastic insert with a bullet-shaped tip that protrudes from the tracheostomy tube
- Used to facilitate tube insertion and must be removed in order to ventilate
What are the features of a standard tracheostomy outer tube?
- Curved or angled (110° to 135°) tube to conform closely to the anatomy of the trachea
- Often have a tapered tip to aid insertion
- Square cut tip (not bevelled) to reduce the risk of obstructing the tube against the wall of the trachea
- 15mm connector is attached to allow the tracheostomy tube to be attached to a breathing circuit for ventilator support
- May be found on the inner tube on certain types of tracheostomy
- Creates a seal to facilitate positive pressure ventilation and prevent from aspiration
- High-volume low-pressure cuffs most commonly used
- Allows tube the tube to be fixed in place by ribbons tied around the patients neck or by sutures
- Linked via an integrated channel to a small hole in the shaft of the tube above the cuff
- Allows secretions that pool above the cuff to be removed by suction
What are the components of a typical tracheostomy tube?
- Rigid at insertion and softens at body temperature to accommodate to individual patient’s anatomy
- High degree of biocompatibility
- Prone to retention of bacteria and is therefore for single use
- Excellent water and chemical resistance
- Reduces adherence of secretions and bacteria reducing biofilm layer
- Promotes easier passage for mucus
- Sterilizable but confined to single patient use
- Cost effective for long-term use
- Rigid at insertion and softens at body temperature to accommodate to individual patient’s anatomy
- Secretions are less likely to adhere to the tube, making it easier to clean
- Some antibacterial property
- Cost effective in long term (changed every 5 years)
- Easily conforms to the anatomy
- Offer great comfort and flexibility
- Lack sufficient rigidity
- Autoclavable but confined to single patient use
- Soft and flexible but stable
- Prevents kinking and compression
Classification & Selection
How can the types of tracheostomy tubes be classified?
- A variety of tubes are available with different characteristics
- Tubes may be classified based upon:
- Material
- Internal diameter
- Length (fixed or variable)
- Presence of a cuff
- Presence of fenestrations
- Presence of a subglottic suction port
- Presence of an inner cannula
How do you decide upon the correct tracheostomy tube for a patient?
- Should be chosen to suit the individual patient:
- Must be a multidisciplinary decision
- Type should be re-evaluated continually as patients needs may change
- Considerations include:
- Tubes with sub-glottic suction port useful in patient with secretions. They are recommended as standard in critical care patients as part of standard VAP intervention bundle
- Cuffed tubes help prevent aspiration of secretions or gastric contents and should be used in patients that are unable to manage secretions
- Fenestrations increase the risk of oral or gastric secretions entering the lungs and should not be used in those at risk of aspiration
- Standard tubes may be unsuitable in abnormal anatomy
- Obese patients may require tube with extended proximal length (adjustable flange)
- Patients with fixed flexion deformity may not accommodate tubes with a fixed angulation
- Pathology such as tracheomalacia or granuloma formation may necessitate the use of a tracheostomy tube that has a longer distal length
- Patient who are being 'weaned' may benefit from tubes that are a uncuffed or smaller in size than initially inserted
- Allows greater gas flow, increased ease of vocalisation and laryngeal rehabilitation
- Tubes with a cuff and without fenestrations are required to facilitate positive pressure ventilation
- Though single cannula tubes may necessitate disconnection from ventilation to clean the tube, they are generally recommended in critical care to reduce the risk of tube obstruction particularly as respiratory support reduces
Tube Size
How are tracheostomy tubes sized?
- Most are sized by internal diameter in millimetres (mm):
- May not take account of the inner cannula in all cases
- Tubes from different manufacturers with the same internal diameter may have quite different external diameters and length
What is the ideal size of a tracheostomy tube for a patient?
- Should be individualised according to the patient and clinical situation:
- Ideal size requires a tube with an outer diameter 2/3rds to 3/4rs the inner calibre of the patient’s trachea at the point of insertion
- May be a role for pre-procedural ultrasound or imaging in tube selection
- There are advantages and disadvantages to large and small calibre tubes:
- Reduces airway resistance and required pressures
- Easier for spontaneous ventilation
- Easier to facilitate suctioning and bronchoscopy
- Limit airflow to the glottis for vocalisation when the cuff is deflated
- Require wide stomas
- Prohibit adequate cuff inflation to cushion the rigid tube from the tracheal mucosa
- Allow greater airflow to the glottis for vocalisation when the cuff is deflated
- May decrease the incidence of tracheal stenosis
- Present difficulties in airway suctioning and bronchoscopy
- Harder for spontaneous ventilation
- Require high intracuff pressures which can damage mucosa
Tube Length & Adjustable Flange Tubes
What are the dimensions of a standard tracheostomy tube?
- Tracheostomy tube length varies with type (12-20cm) and is available in:
- Standard length (12-14cm) – for those with normal airway anatomy
- Longer Length:
- Extended proximal length – for those with deep-set tracheas
- Extended distal length – for those with tracheal problems
- Adjustable flange (20cm) – flexible angulation and length
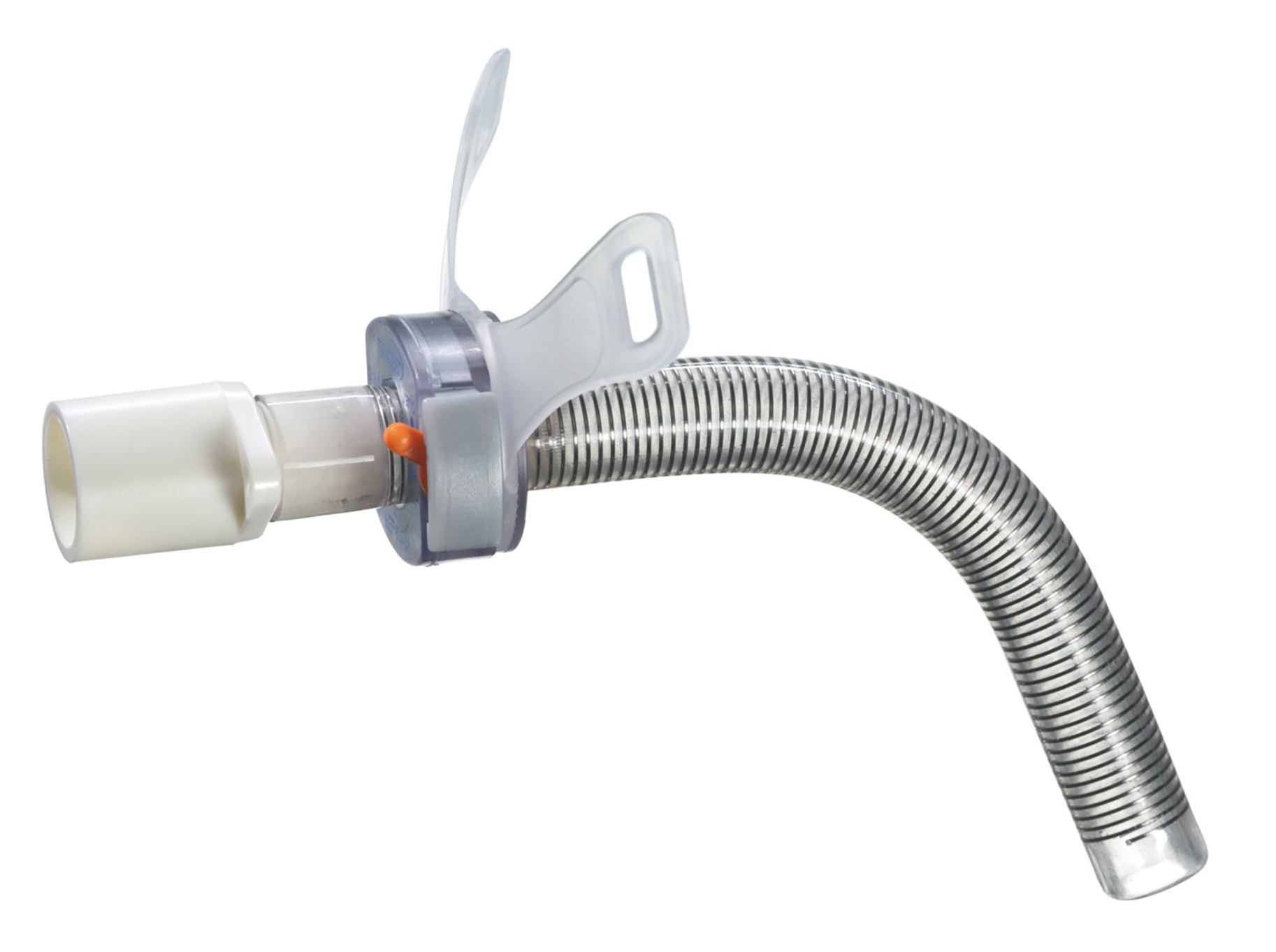
What is an adjustable flange tracheostomy?
- Reinforced tube that allows the length of the tube to be adjusted:
- Altered through a locking mechanism located at the flange
- Allows variable length to be left within the trachea
- Can be used to account for individual patient factors such as obesity or a neck mass
- NCEPOD report suggested should be used in around 30% of intensive care admissions, based on BMI
- Care must be taken to secure the flange to the tube to ensure that it does not move
- If accidentally opened can lead to displacement of the tube
Single & Dual Cannula Tubes
What are single and dual cannula (lumen) tracheostomies?
- Has a removable thin flexible sleeve (inner cannula) that fits directly inside the outer tube
- Some designs require inner cannula to the breathing system via a standard 15 mm connector
- Involves a single outer tube only
What are the differences between single and dual cannula (lumen) tracheostomy tubes?
- Generally preferred in adult patients (inherently safer) and recommended in those on lower respiratory support
- Permits the lumen to be cleaned to prevent blockage
- Reduces the risk of airway obstruction from retained secretions
- Reduces the frequency of tracheostomy tube change from 7-10 days to >28 days
- The presence of an inner cannula reduces the internal diameter of the airway
- May increase the resistance to movement of air and increase the work of breathing, contributing to weaning difficulty
- Necessitates repeated circuit disconnection to facilitate inner cannula exchange
- Most common in paediatric patients
- May be useful in adults with high respiratory support requirements on humidified closed circuits (benefits of removable cannula may be less marked)
- May reduce the resistance to movement of air and decrease the work of breathing
- Reduces circuit disconnections for tube exchange
- Higher risk of blockage and airway obstruction
- Necessitates external tube change every 7-10 days
Cuffed & Uncuffed Tubes
What are the differences between cuffed and uncuffed tracheostomy tubes?
- Patients receiving positive pressure ventilation
- Patients who are at high risk of aspiration
- Creates a seal to allow delivery of positive pressure ventilation
- Protects the lungs from gastric and upper airway secretions
- Can still allow for vocalisation through deflation of the cuff
- Little or no voicing occurs when the cuff is inflated
- Risk of mucosal injury and stenosis at the site of the cuff
- Patients who can protect their own airway, have an adequate cough reflex and can manage their secretions
- Frequently used for patients being cared for in the community
- Removes the risk of tracheal damage caused by inflation of the cuff
- May aid swallowing
- May aid communication with the concomitant use of a speaking valve
- Unable to prevent aspiration of secretions
- Cannot be used for the delivery of positive-pressure ventilation
Fenestrated & Unfenestrated Tubes
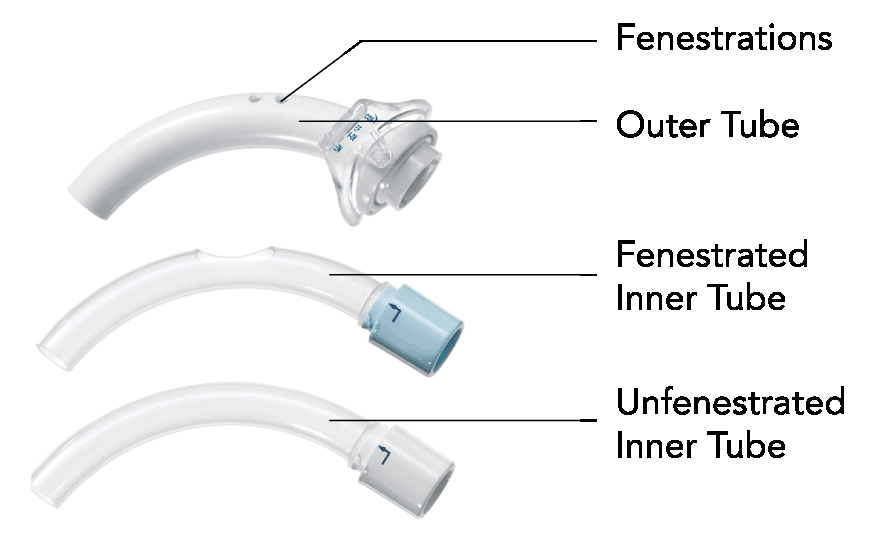
What are tracheostomy tube fenestrations?
- Multiple small holes in the greater curvature of the tracheostomy shaft
- Allows air to pass through the patient’s oral/nasal pharynx as well as via the tracheostomy tube
- Enables the patient to speak and produces a more effective cough.
- By using different inner cannulae) the outer hole can be blocked or remain patent.
What are the differences between fenestrated and unfenestrated tracheostomy tubes?
- Patients receiving positive pressure ventilation
- Patients who are at high risk of aspiration
- Creates a channel to allow delivery of positive pressure ventilation
- Protects the lungs from gastric and upper airway secretions
- Can still allow for vocalisation through deflation of the cuff
- Little or no voicing occurs when the cuff is inflated
- Increases airflow resistance compared to unfenestrated tubes, particularly when tube is capped
- Spontaneously breathing patients imminently approaching decannulation (useful when unable to manage capping of unfenestrated tube)
- Generally not recommended when cuff inflation is still required to protect the airway from aspiration
- Allows maximum airflow to upper airway for voicing when tracheostomy occluded (speaking valve or cap)
- Allows some airflow to vocal cords for speech even when cuff inflated
- Reduces airflow resistance and work of breathing when appropriately sited
- May still be used for positive pressure ventilation if an unfenestrated inner cannula is placed (not recommended in newly formed stoma as air may still leak around fenestrations, risking surgical emphysema)
- Fenestrations increase the risk of oral or gastric contents entering the lungs
- Positive pressure ventilation will result in air leak and should be avoided where possible
- There is a risk of surgical emphysema in patients with newly formed tracheostomies
- May stimulate granuloma formation around the fenestrations
- Requires placement of an unfenestrated inner cannula when undertaking suctioning
Subglottic Ports
What are sub-glottic suction tubes?
- Sub-glottic suction tubes have a system integrated to allow suction of secretions that pool above the cuff:
- Small hole located in the shaft of the tube above the cuff and below the vocal cords
- Channel runs up inside the endotracheal tube
- Connected to a suction port external to the tube
- Secretions can be removed by continuous or intermittent suction
- Evidence suggests they are useful in reducing the rate of ventilator-associated pneumonia (VAP)
- Can also be used to provide an external flow of gas to the glottis for above cuff vocalisation