RESOURCES
OBJECTIVES & QUESTIONS
Overview of Obstruction and Displacement
How common are tracheostomy emergencies?
- Reported incidence of tracheostomy displacement varies widely
- Rates of accidental displacement in critical care reported between 0.35% and 15%
- In a NPSA 2 year report of critical care patients with tracheostomies:
- 453 incidents were reported
- 338 incidents led to harm
- 15 incidents contributed to death
- 60% were due to blocked or displaced tracheostomies
What are the risk factors for accidental tracheostomy decannulation?
- Mental status change
- Traumatic brain injury
- Increased secretion load
- Recent tracheostomy change
- Percutaneous insertion technique
- Increased neck thickness
- Paediatric age group
How does the age of the tracheostomy affect the ability to replace a decannulated tube?
- Most concerning because of the lack of mature stoma formation and narrower tract:
- Increases the risk of airway loss
- Replacement should be attempted only with direct visualization via fibreoptic endoscopy:
- Reduces the risk of creating a false passage into the soft tissue
- If unavailable or is unsuccessful oral intubation may be necessary
- Often easier to replace as stoma matured
- Important not to delay as even a mature stoma may significantly narrow over the course of hours making delayed recannulation more challenging
- Regardless of the age of the tracheostomy, if resistance is met, a smaller tracheostomy tube should be selected and insertion reattempted
- If recannulating is unsuccessful, bag-valve ventilation and oral intubation may be necessary if the patient fails to oxygenate or ventilate
What are the causes of tracheostomy obstruction?
- Small tracheostomy tube size
- Single cannula tracheostomy tube
- Poor tracheostomy care
What are the risk factors for tracheostomy tube obstruction?
- Dried secretions
- Mucous plugs
- Clotted blood
- Partial tube displacement
- Partial impingement by the posterior tracheal wall
- Granulation tissue build-up
- Displacement of the tracheostomy into a false lumen
What are the ‘red flag’ signs of impending tracheostomy displacement or obstruction?
- Increasing ventilatory support or increasing oxygen requirements
- Respiratory distress or difficulty in breathing
- Sudden ability to talk (implying the cuff no longer ‘sealing’ the trachea)
- Frequent requirement for inflation of the cuff to prevent air leak
- Pain at the tracheostomy site
- Subcutaneous emphysema
- Suction catheter not passing easily into the trachea
- Changing, inadequate or absent capnograph trace
- Suspicion of aspiration
Management of Tracheostomy Obstruction or Displacement
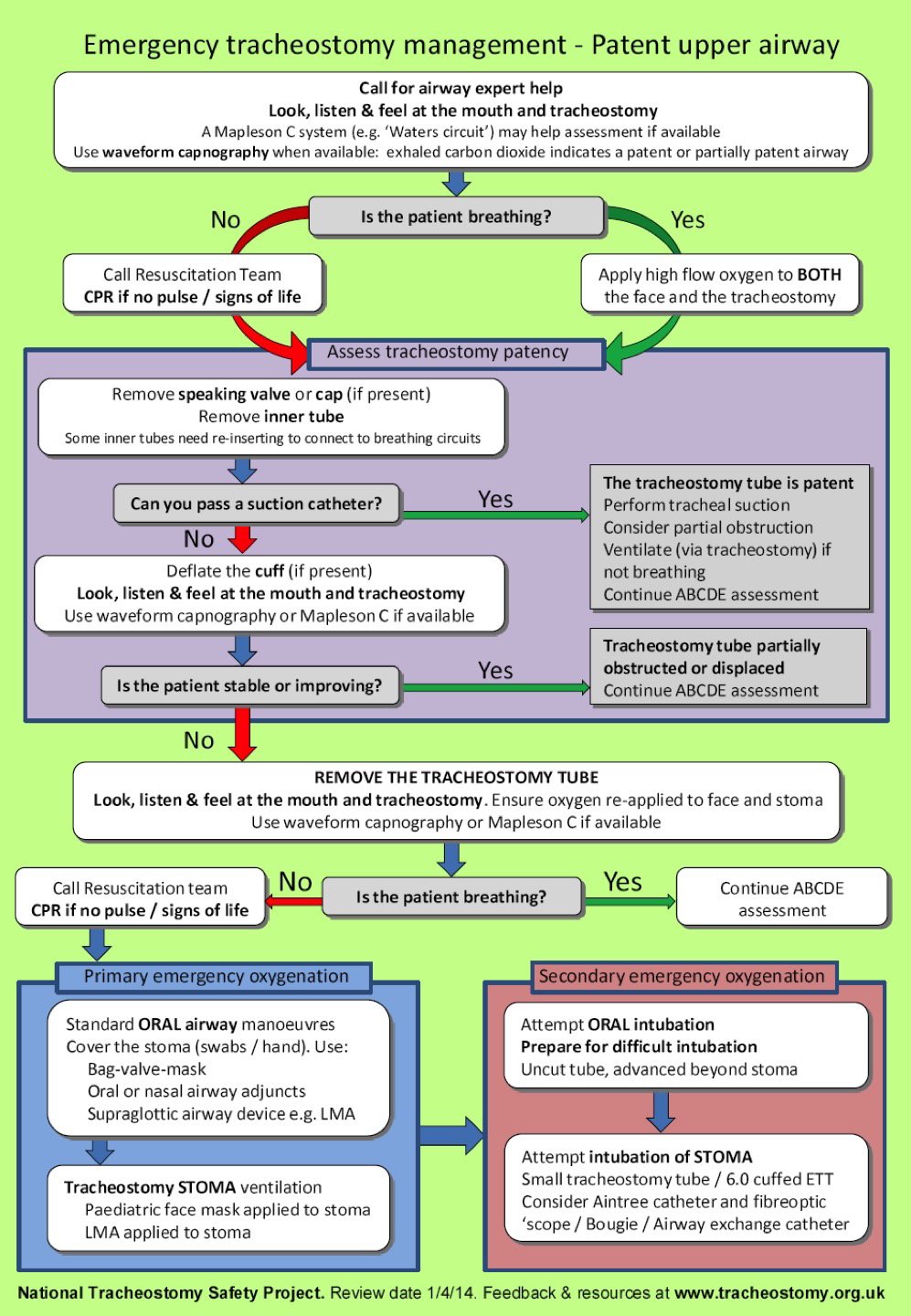
What is the stepwise approach to a tracheostomy emergency?
- Call for airway expert help
- Assess the tracheostomy quickly:
- Look, listen & feel at the mouth and tracheostomy
- Use a ‘Waters circuit’ and capnography if available
- If not breathing call for the emergency team and commence CPR if no signs of life
- If breathing apply oxygen to both the mouth and tracheostomy
- Assess the tracheostomy patency:
- Remove inner tube and any valves / caps
- Try to pass a suction catheter
- If unable to pass a catheter deflate cuff
- If not improving remove the tracheostomy tube
- If breathing and stable continue assessment
- If not breathing call arrest team and attempt primary means of oxygenation
- Primary attempts at oxygenation:
- Standard oral airway manoeuvres / LMA with stoma covered
- LMA or paediatric facemask applied to stoma
- Secondary attempts at oxygenation if still unsuccessful
- Oral intubation with uncut tube past stoma
- Stoma intubation:
- Size 6.0 ETT over bougie
- Consider fibreoptic scope and Aintree catheter as first line
Management of Laryngectomy Obstruction or Displacement
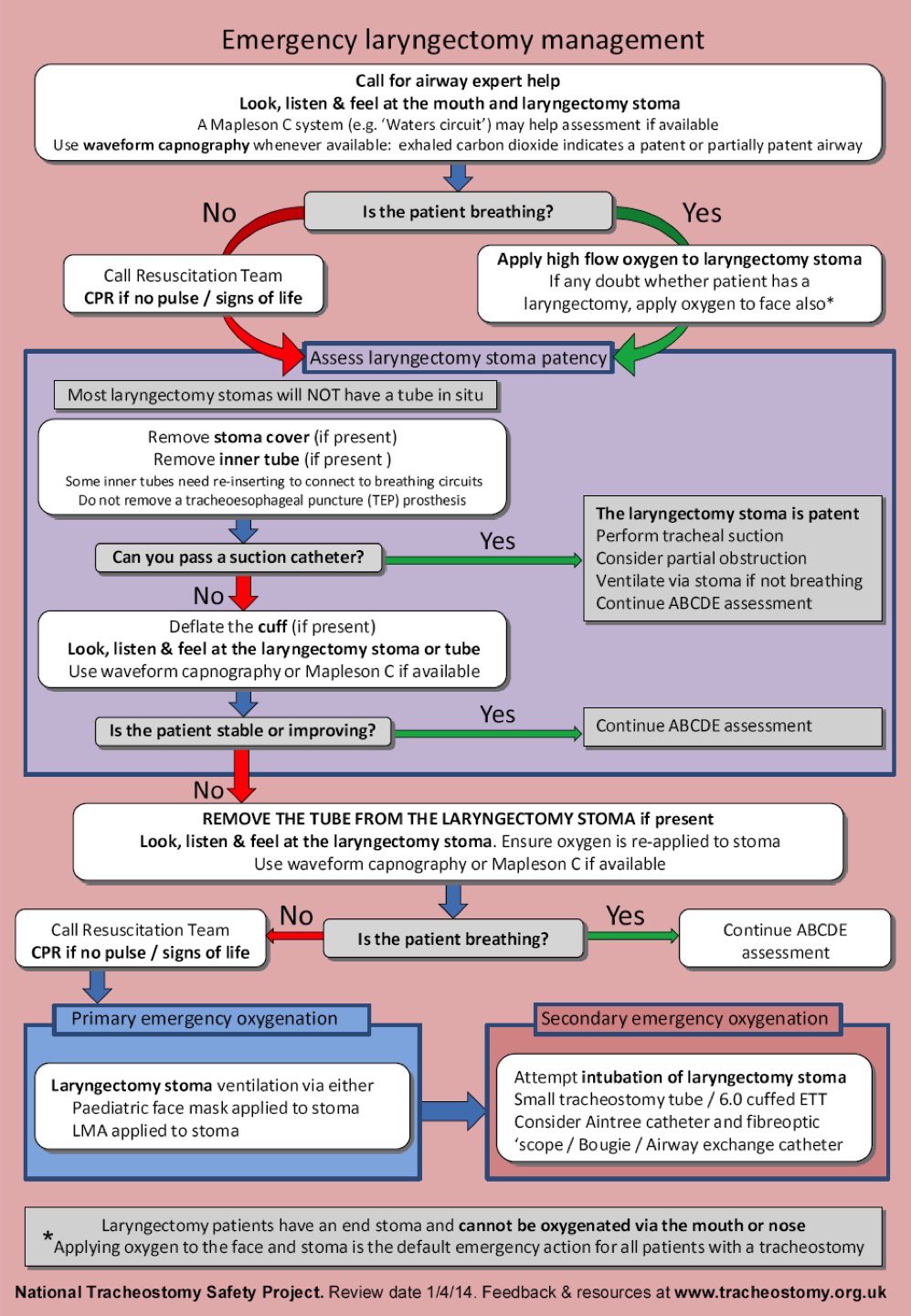
What is the stepwise approach to a laryngectomy emergency?
- Call for airway expert help
- Assess the laryngectomy quickly:
- Look, listen & feel at the mouth and laryngectomy
- Use a ‘Waters circuit’ and capnography if available
- If not breathing call for the emergency team and commence CPR if no signs of life
- If breathing apply oxygen to the laryngectomy stoma (and mouth if in doubt of stoma type)
- Assess the laryngectomy patency:
- Remove inner tube and any valves / caps
- Try to pass a suction catheter
- If unable to pass a catheter deflate cuff
- If not improving remove the laryngectomy tube
- If breathing and stable continue assessment
- If not breathing call arrest team and attempt primary means of oxygenation
- Primary attempts at oxygenation:
- LMA or paediatric facemask applied to stoma
- Secondary attempts at oxygenation if still unsuccessful
- Stoma intubation:
- Size 6.0 ETT over bougie
- Consider fibreoptic scope and Aintree catheter as first line
- Stoma intubation:
Overview of Bleeding
How common is bleeding following tracheostomy?
- NCEPOD 2014 report highlighted a rate of:
- Major bleeding: 1.2%
- Minor bleeding: 4.4%
What are the causes of bleeding from a tracheostomy?
- Bleeding from surgical site (most common)
- Irritation from suctioning/ manipulation
- Tracheitis
- Granulation tissue
- Infection of stoma site/ tracheitis
- Tracheo-innominate artery fistula (life-threatening cause)
- Blood from lungs, upper airway, or GI tract
- Bleeding diathesis
What is tracheo-innominate artery fistula (TIAF)?
- The most feared haemorrhagic complication of a tracheostomy:
- Incidence of approximately 0.7% of patients with tracheostomy
- Mortality is greater than 90%
- Occurs due to the development of a direct connection between the trachea and the innominate artery branch of the aorta
Why does tracheo-innominate fistula develop?
- Tracheal tube can cause pressure on the anterior wall of the trachea
- Results in mucosal ischemia and fistula formation with the posterior wall of the innominate artery:
- Commonly involved as crosses behind the trachea at the 9-12th tracheal rings
- Within range of the tip of the tracheostomy tube
- Risk is increased with:
- Cuffed tracheostomy tube
- Low tracheostomy placement
- High cuff pressure
- High riding innominate artery
- Excessive neck movement
- Tracheostomy infection
When should tracheo-innominate artery fistula (TIAF) be considered?
- NCEPOD 2014 report highlighted a rate of:
- Major bleeding: 1.2%
- Minor bleeding: 4.4%
How do you assess a possible tracheo-innominate artery fistula (TIAF)?
- NCEPOD 2014 report highlighted a rate of:
- Major bleeding: 1.2%
- Minor bleeding: 4.4%
Management of Bleeding
How do you assess a possible tracheo-innominate artery fistula (TIAF)?
- R
- A
- R
- A

