RESOURCES
Guidelines
- Consensus (2017) – Consensus guidelines for lumbar puncture in patients with neurological diseases
- ABN (2018) – Guidelines for lumbar puncture and bleeding risk
Review Articles
OBJECTIVES & QUESTIONS
Indications & Contraindications
What are the indications for performing a lumbar puncture?
Diagnostic
- Investigate meningoencephalitis
- Investigate neurological disorders:
- Multiple Sclerosis
- Guillain Barre
- Mitochondrial Disorders
- Paraneoplastic Syndromes
- Investigate subarachnoid haemorrhage
- Investigate disorders of intracranial pressure
- Administer diagnostic agents:
- Contrast media in myelography
Therapeutic
- Spinal anaesthesia
- Administer therapeutic agents:
- Intrathecal chemotherapy
- Intrathecal antibiotics
- Intrathecal baclofen
- Manage specific disorders:
- Benign intracranial hypertension
- Acute communicating hydrocephalus
- Cryptococcal meningitis in HIV infection
- CSF leak
What are the contraindications to performing a lumbar puncture?
Absolute
- Space occupying lesion with mass effect and evidence of increased ICP:
- Risk of cerebral herniation
- Suggested by midline shift or loss of cisterns on CT
- Posterior fossa mass
- Arnold-Chiari malformation
- Coagulopathy (see BSN Guidance):
- Platelets <40,000
- INR >1.4
- Anticoagulant & antiplatelet medication
- Skin infection at puncture site
- Patient refusal
Relative
- Brain, spinal and epidural abscess
- Issues with positioning:
- Respiratory distress
- Cardiovascular instability
- Poor mobility
- Spinal anomalies:
- Congenital anomalies
- Previous surgery
- Degenerative disease
Who should have a CT prior to an LP?
- Focal neurological defecit
- Papilledema
- Reduced consciousness (GCS<12)
- Immune compromise
- Previous CNS disease
- Recent seizures
Complications
What are the complications of lumbar puncture?
Immediate
- Failure
- Bloody tap
- Nerve root pain
Early
- Post-dural puncture headache (PDPH)
- Post-dural puncture herniation (very rare)
- Spinal / epidural haematoma
- Spinal cord ischaemia
- Nerve damage (temporary or permanent)
- Infection:
- Local injection site
- Epidural abscess
- Meningitis (rare)
Late
- Post-LP Back pain
- Epidermoid tumour
What is post-dural puncture headache PDPH?
See section: Post-Dural Puncture Headache
What are the risk factors for PDPH following lumbar puncture?
Patient Related
- Younger age (<40)
- Female gender
- History of PDPH
- Chronic or recurrent headache
- Fear of post-LP complaints
Procedure Related
- Wide bore needle (<25G)
- 'Traumatic' cutting bevel needle tip
- Active withdrawal of CSF
- Sitting position
- Large volume fluid collection
- Multiple attempts
Positioning & Puncture Site
Which position should the patient be placed for a lumbar puncture?
- Correct positioning is key to procedural success
- Two positions are can be used for lumbar puncture:
Positioning
Comments
Lateral Recumbent
- Left lateral position (for a right handed operator) with back along the edge of the bed
- Head propped up on a single pillow to maintain a straight spine
- Knees, hips and neck flexed in the foetal position to optimise interlaminar foramen
- Hips and shoulders should lie vertically above each other
- First-line position for performing lumbar puncture
Sitting
- Sit patient on edge of bed with feet resting on a stool
- Flex trunk by having patient lean forward clasping a pillow
- CSF pressure cannot be reliably measured in the sitting position
- May be useful in patients with respiratory compromise
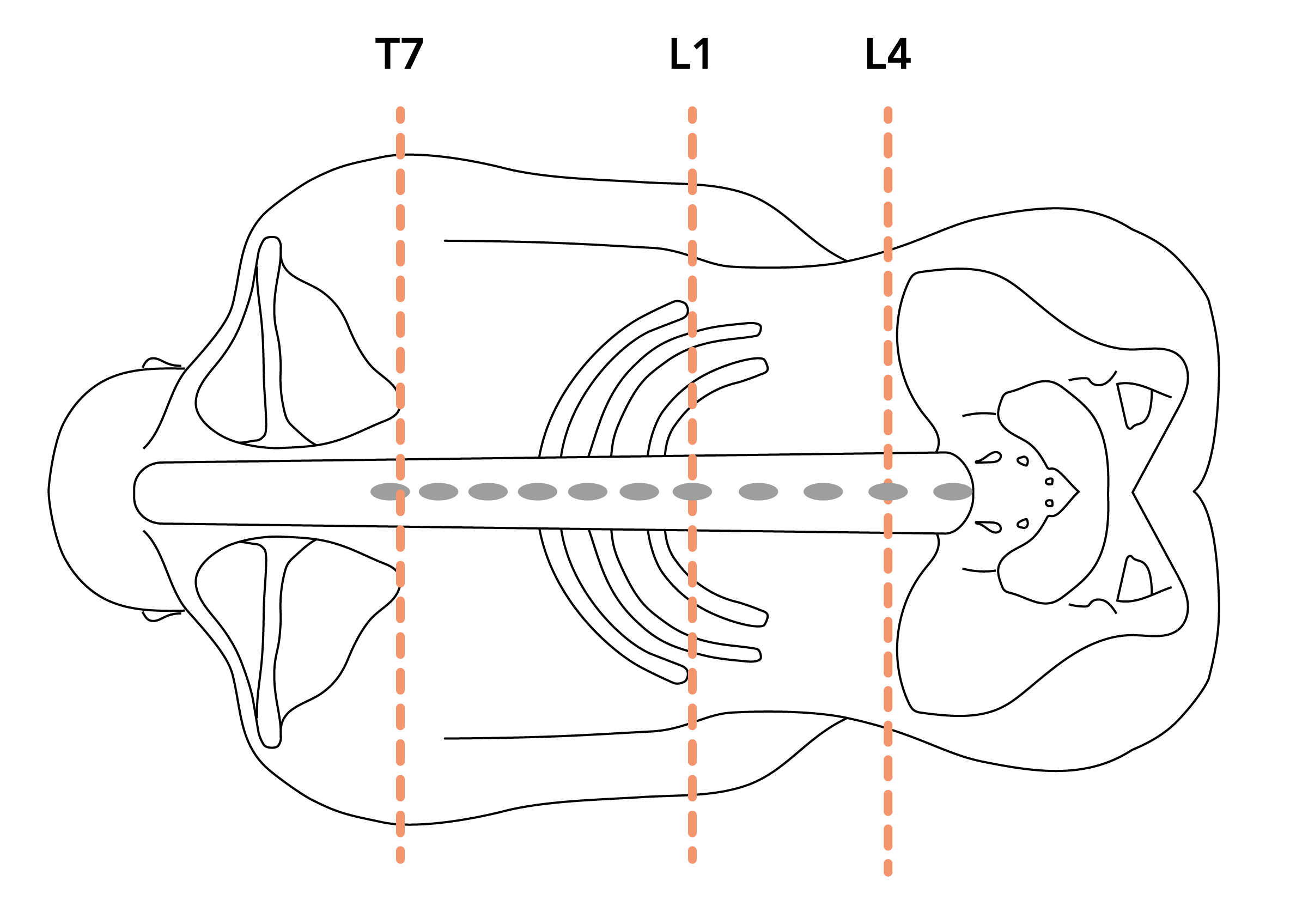
Which interspace should a lumbar puncture be performed at and how can this be identified?
- Lumbar puncture should not be performed at or above the L2/3 interspace:
- In adults, the solid spinal cord ends at L1 (ranges from T11 to upper L3)
- At this level the conus medullaris continues distally as the cauda equina
- Puncture above this level risks damaging the cord
- The L4/5 or L3/4 interspace is usually used
- The L4 spinous process can be estimated using Tuffier’s line:
- An imaginary line drawn between the iliac crests
- Significant anatomical variation exists between patients
- Alternative anatomic landmarks include:
- The tip of the scapula in line with T7 spinous process
- The tip of the 10th rib in line with L1 spinous process
Procedure
How do you perform a lumbar puncture?
- Sterile gloves
- Sterile gown
- Hat and mask
- Sterile Drape
- Chloraprep x2 (with 0.5% chlorhexidine)
- Lidocaine
- Syringe
- 22G and 24G needle
- Sterile gauze
- Spinal Needle (22-25G atraumatic)
- Manometer (40cm)
- 3-way tap
- Specimen pots x4
- Dressing
Key Considerations
– Risk Assessment
– Consent
– Positioning
Risk Assessment
- Confirm no undue bleeding risk:
- Check coagulation and platelet screen
- Confirm anticoagulant and antiplatelet medication stopped appropriately
- Assess need for CT head prior to LP
Consent
- Explain the risks of the procedure and complete a consent form
- Complete a consent form 4 for ventilated patients
Positioning
- Position the patient in the lateral recumbent position:
- Knees to chest and back flexed as far as possible
- Ensure one hip exactly above the other
- Identify insertion site at L4/5 interspace:
-
- L4 in line with the top of the iliac crests (Tuffier’s line)
- L3-4 interspace above may be used as an alternative

-
- Prepare sterile LP tray
- Ensure sterile technique:
- Wash hands thoroughly
- Put on sterile gloves, gown, mask, and hat
- Ensure sterile skin and surface:
- Using chlorhexidine 0.5% to clean the skin at the insertion site
- Allow to air dry
- Drape the patient
- Infiltrate the skin and subcutaneous tissue with 1% lidocaine with a 25-gauge needle.
- If using a narrow gauge spinal needle Insert the introducer needle:
-
- Direct the needle on a 10-degree angle toward the umbilicus
- Should be introduced no more than 2/3-3/4 of the total length
-
- Insert the spinal needle and advance the needle slowly, removing the stylet every 2-3 mm to check for CSF flow:
- Bevel should always enter facing upwards
- A tactile click is usually felt as the needle tents and passes through the dura
- If the patient complains of nerve root pain: Do not advance the needle, withdraw 2 mm, remove stylet and check for CSF. If none, then replace the stylet and remove
- Measure CSF pressure if required:
- Rotate the needle 90 degrees counter-clock wise
- Add 3 way stop-cock with tap closed to patient
- Add monometer and open stopcock
- Collect CSF sample
- Remove 1-2ml of CSF in each of the four tubes
- Active CSF withdrawal using a syringe should only be performed when a patient cannot tolerate a long procedure.
- Send samples to the lab as indicated.
- Turn needle 90-degrees clockwise and replace stylet prior to removal
- Cover with sterile dressing
- Document the procedure in the patients notes
- Assess patient for adverse reactions to procedure
- Inform patient to monitor for signs of bleeding or infection
- Post procedural analgesics as needed
- Bed rest and oral fluid not specifically advised
Tests & Samples
Which investigations are performed on CSF?
Routinely Performed
- Opening pressure
- Total Cell count (WBC & RBC)
- Cell differential count
- Glucose (CSF/plasma ratio)
- Total protein
Useful in Specific Situations
- Microbiological stains:
- Gram stain
- Acid-Fast stain
- Microbiological cultures:
- Bacterial culture
- Fungal culture
- TB culture
- Microbiological Antigens:
- VDRL
- Pneumococcus / meningococcus
- Cryptococcus
- Aspergillus
- Toxoplasmosis
- Viral PCR
- Viral culture
- Lactate
- Electrophoresis
- Cytologic examination
- Specific proteins (CRP, Tau, B-amyloid)
Which samples should be collected for analysis and how much CSF is required?
- A general consensus is to label sample tubes sequentially from an LP
- These can then be used for:
1st
- Minimum 3 drops
- More as able up to 0.5ml*
- Total protein
- Glucose
- Other biochemistries
2nd & 3rd
- Minimum 3 drops (6 for cryptococcus)
- More as able up to 2.5ml*
- Cell count & differential
- Microbiological stains
- Microbiological cultures•
4th
- 20 Drops
- 1ml*
- Xanthochromia (Protect this sample from the light by placing it in a thick brown envelope outside the usual plastic specimen bag)
- *1mL is about 20 drops from the Luer connector on a needle
- A serum sample must be sent simultaneously for glucose and oligoclonal bands
What are the considerations for commonly performed CSF investigations?
Routinely Performed
Volume
Laboratory
Considerations
Microbiology (Bacteriology, TB, cryptococcus)
>3 drops (6 drops for cryptococcus) but as much as is practically possible
Microbiology
- Increased sensitivity with higher volumes of CSF
Viral PCR & Culture
>4 drops but as much as is practically possible
Virology
- Increased sensitivity with higher volumes of CSF
Biochemistry
>3 drops but more if practically possible
Biochemistry
- Send paired serum protein and glucose samples
Xanthochromia
20 drops
Biochemistry
- Transport in opaque envelope or wrap sample container in foil.
Oligoclonal Bands
20 drops
Immunology
- Send paired serum serology sample
Cytology
50 drops or as much as is practically possible
Neuropathology
- Ensure swift transport to laboratory
Lactate
20 drops
Biochemistry
- Send paired serum lactate sample
Spinal Needles
What are the key features of spinal needles?
- Available in a variety of lengths:
- Standard length is 75mm
- Long needles (90mm) are available for obese patients
- Available in variety of diameters (22-27G)
- Smaller needles produce less damage to the dura and have a lower rate of PDPH
- Larger needles have better flow rates making pressure measurements easier
- Current consensus is that needle gauges of 22-25 are preferred for LP
- Needle tip may be ‘cutting’ or ‘atraumatic’ in design
- Introducer used with needles 25G and finer
- Stylet used to prevent coring of tissue on insertion
- Transparent needle hub allows early identification of CSF
What types of needle tips are available on spinal needles and what are their advantages and disadvantages?
Needle Type
Examples
Advantages
Description
Cutting
Quincke
Atraucan
Atraucan
- Cuts through tissue and ligaments, making insertion easier
- Aperture at the tip of the needle, so less likely to straddle the dural membrane if injecting medication - reduces the risk of failed spinals
- Higher incidence of PDPH
- Cutting tip potentially increases the risk of nerve damage
- Less tactile feed back as it passes through the dura
- Risk of tissue coring and aperture occlusion as no stylet is used
Atraumatic
Sprotte
Whitacre
Ballpen
Whitacre
Ballpen
- Separates the longitudinal fibres of the dura without cutting them, causing less trauma
- Reduces CSF leakage and hence PDPH rates
- Generates a more convincing ‘click’ on breaching the dura
- Small orifice increases resistance to CSF aspiration and injection
- Orifice usually sits proximal to the tip and may straddle the dural membrane leading to failed spinal
What types of atraumatic spinal needles are commonly available for lumbar puncture and what are their advantages and disadvantages?
Needle Type
Profile
Description
Advantages
Description
Whitacre
- Solid conical blunt tip
- Rectangular lateral aperture just proximal to tip
- Small lateral orifice increases resistance to CSF aspiration and anaesthetic injection
- The orifice sits proximal to the tip, and may straddle the dural membrane, increasing the risk of spinal failure by inadvertent injection into the epidural space.
Sprotte
- Tapered blunt tip
- Lateral aperture is larger, oval shaped and sits further from the tip than the Whitacre
- Larger aperture for faster backflow of CSF into the hub on entering the subarachnoid space.
- Less resistance to injection and aspiration
- Tapered tip allows gradual and less traumatic separation of dural fibres, reducing PDPH rates compared to Whitacre needles
- The lateral aperture is larger and a greater distance from the tip compared to the Whitacre - increases the risk of straddling the subarachnoid and epidural space at the time of injection and raising the likelihood of a failed or partial block
Ballpen
- Sharp stylet within the lumen of the hollow spinal cannula
- Unlike other stylets, it protrudes 2–3 mm from the distal end of the spinal cannula with a smooth junction between the two.
- Opens at the distal tip of the needle, reducing the risk of injecting into the epidural space, as sometimes occurs with lateral aperture needles
- No problems with coring of tissue or blockage of the aperture
- The distance the needle tip needs to move into the subarachnoid space before CSF is seen is less, theoretically reducing the risk of neurological damage compared to Whitacre and Sprotte needles
- Withdrawal of the stylet may dislodge the hollow cannula from the subarachnoid space
What types of cutting spinal needles are available for lumbar puncture and what are the advantages and disadvantages?
Needle Type
Profile
Description
Advantages
Description
Quincke
- Diamond-shaped cutting bevel and an opening at the tip
- Cuts through tissue and ligaments, making insertion easier
- Aperture at the tip of the needle, so less likely to straddle the dural membrane - reduces the risk of failed spinals
- Higher incidence of PDPH (8% vs. 3% for a 25G Whitacre needle)Cutting tip potentially increases the risk of nerve damage
- Higher incidence of PDPH (8% vs. 3% for a 25G Whitacre needle)
- Cutting tip potentially increases the risk of nerve damage
- Less tactile feed back as it passes through the dura
Atraucan
- Double-bevel with a sharp initial bevel for creation of incision and a second bevel for the dilation of tissues
- Causes less leakage of cerebrospinal fluid than Quincke needles
- Aperture at the tip of the needle, so less likely to straddle the dural membrane - reduces the risk of failed spinals
- No strong evidence that PDPH rates are comparable to atraumatic needles
- May be associated with higher rates of post
Applied Anatomy
Which layers does a needle pass through during lumbar puncture?
- Skin
- Subcutaneous fat
- Supraspinous ligament
- Interspinous ligament
- Ligamentum flavum
- Epidural space
- Dura mater
- Arachnoid mater
- Subarachnoid space
Where does the spinal cord end?
- Spinal cord ends at the conus medullaris
- Level of conus traditionally considered to be lower in infants and children than adults – studies suggest median level is similar
- Level of the conus medullaris varies significantly between individual patients:
Adults
Infants
Upper Range
T11
T12
Median
L1
L2
Lower Range
L3
L4
Which surface landmarks can be used to identify vertebral levels?
- The L4 spinous process can be estimated using Tuffier’s line:
-
- Significant anatomical variation exists between patients
- An imaginary line drawn between the iliac crests
- Alternative anatomic landmarks include:
- The tip of the scapula in line with T7 spinous process
- The tip of the 10th rib in line with L1 spinous process