OBJECTIVES & QUESTIONS
Introduction & Definitions
How is diarrhoea defined?
Defined by ‘The World Health Organisation’ as:
The passage of three or more loose or liquid stools per day, or more frequently than is normal for the individual
How is faecal incontinence defined?
Defined by ‘The Royal College of Physicians’ as:
The involuntary or inappropriate passage of faeces
Recently defined by consensus guidelines as:
When a patient experiences at least two episodes of faecal incontinence with diarrhoea – liquid or semi-liquid stool (according to the Bristol Stool chart) – in a 24-hour time period
How common is acute faecal incontinence in the critically ill?
What are the causes of acute faecal incontinence in the critically ill?
- Antibiotics and altered intestinal flora leading to pathogenic colonisation (e.g. c.difficile)
- Enteral feed
- Drugs (including laxatives, NSAIDs, anti-arrhythmic drugs and cholinergic agents)
- Gut hypoperfusion
- Chemotherapy
- Graft-versus-host disease
- Functional factors:
- Impaired cognition
- Decreased mobility
- Altered communication
- Sedation
- Structural factors:
- Frail and elderly patients
- Previous radiation therapy to the pelvic floor
- Colonic resection or anal surgery
Consequences & Complications
What are the potential adverse consequences of acute faecal incontinence in the critically ill?
- Skin breakdown (moisture lesions, excoriations
- Local skin and wound infections
- Line and device-related infections
- Fluid & electrolyte disturbances
- Impaired patient comfort and dignity
Which patients are at risk of developing complications from acute faecal incontinence?
- Risk of skin breakdown in the perineal region
- Moisture lesion, excoriation, pressure ulcer, burn
- Wounds at risk of infection
- Fournier’s gangrene
- Post-op (e.g. skin flap)
- Risk of cross-infection
- C. difficile, MRSA, E.coli, ESBL, CRE
- Enteric infection/enteritis with no isolation facility
- Immobility:
- Severe respiratory failure
- Multiple trauma
- ECMO
- Large-bore access
- Morbid obesity
- Very frequent or long-lasting diarrhoea
- Poor nutritional status
- Patient comfort and dignity
Management
What are the options available for managing acute faecal incontinence?
- Absorbent products (pads, briefs)
- Faecal collectors
- Faecal or bowel management systems
- Rectal catheter with balloon
- Rectal trumpet
- Bulking agents
- Antidiarrhoeal agents (if not infectious)
- Antibiotics (if infectious)
What is the suggested approach to the management of faecal incontinence?
Fundamentals & Equipment
What are bowel management systems?
- Newer medical device systems inserted into the rectal vault and designed to direct, collect, and contain liquid stool from bedbound, immobilised ill patients allowing for perineal skin protection and healing
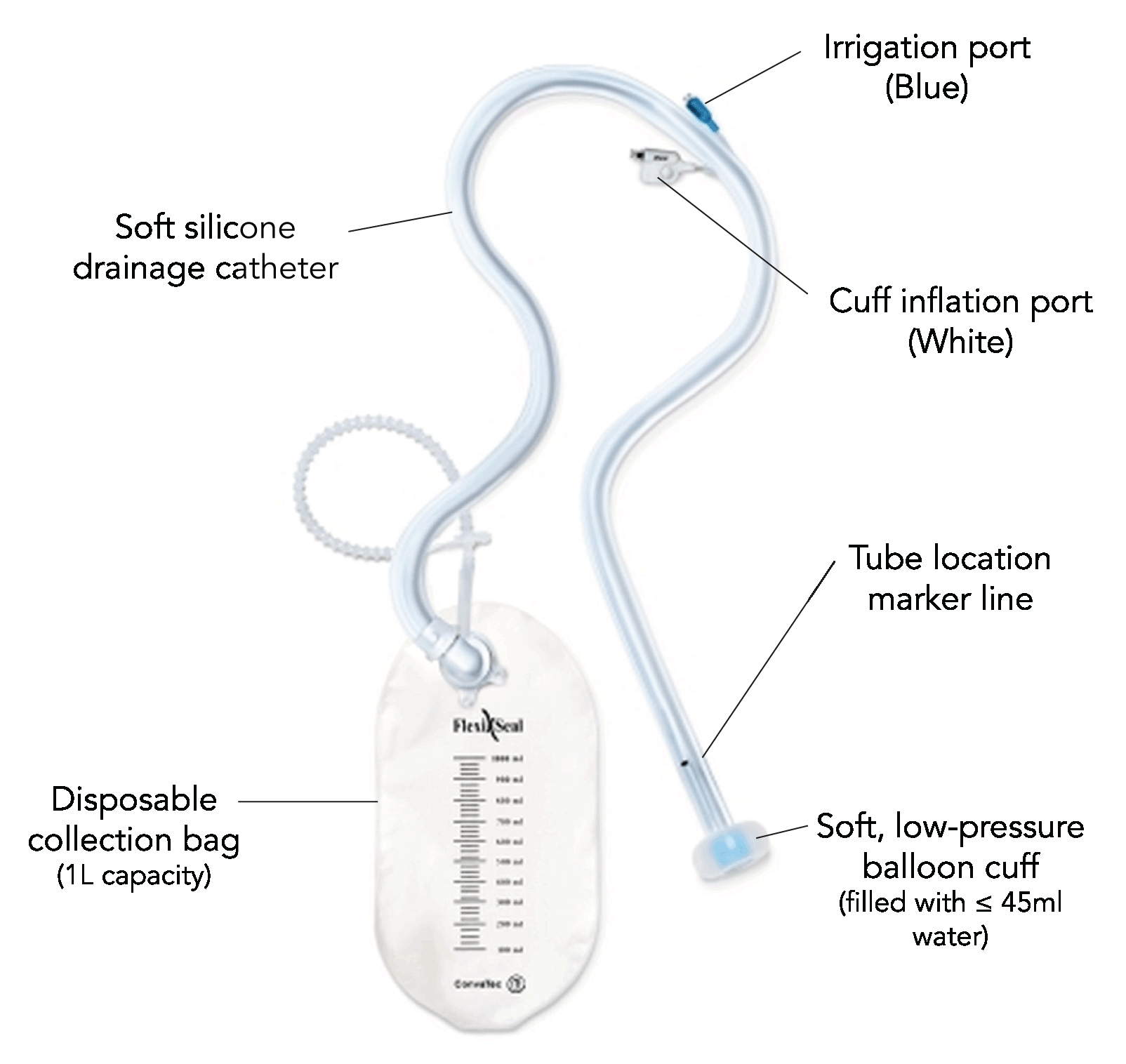
What are the components of a bowel management system?
What are the goals of bowel management systems?
- Reduce the risk of skin breakdown by helping keep the skin clean, dry and free from contaminants.
- Reduce the risk of spread of infection by containing infectious body waste within a disposable, closed system
- Help to protect wounds, surgical sites, and burns from contamination by stool
- Help improve patient comfort
- Help reduce the cost of managing faecal incontinence
- Help maintain patient dignity
Indications & Contraindications
What are the prerequisites for the use of a bowel management system?
- Patients should be bedbound and unable to use toilet facilities
- Stool must be liquid or semi-liquid to drain adequately
- Digital rectal exam should be performed to:
- Exclude faecal impaction
- Determine anal tone (poor tone may increase leakage or contribute to inability to retain the device)
What are the indications for the use of a bowel management system?
Patients who are bedbound with incontinent liquid or semi-liquid stools:
- At risk of perianal and sacral skin breakdown and pressure ulcers.
- Requiring faecal diversion to protect wounds, burns, flaps or grafts.
- Requiring containment of infectious stools
What are the contraindications to the use of a bowel management system?
- Use for more than 29 consecutive days
- Use in paediatric patients
- Faecal impaction
- Suspected or confirmed rectal mucosa impairment (e.g., severe proctitis, ischemic proctitis, and mucosal ulcerations)
- Large bowel (colon) or rectal surgery within the last year
- Rectal or anal injury
- Haemorrhoids of significant size
- Suspected or confirmed rectal/anal tumour
- Any in-dwelling, external rectal or anal device (e.g., thermometer, external faecal collection pouch)
- Allergy to any components within the kit
Caution should be exercised in:
- Bleeding tendencies (anti-coagulant, antiplatelet therapy or underlying coagulopathy)
- Neutropenic sepsis, due to increased risk of proctitis
- Spinal cord injury, due to the possibility of autonomic dysreflexia
- Inflammatory bowel conditions
D
Complications
What are the complications that can occur with the use of a bowel management system?
- Leakage of stool around the device
- Rectal/anal bleeding
- Pressure necrosis
- Ulceration of rectal or anal mucosa
- Perianal skin breakdown
- Temporary loss of anal sphincter muscle tone
- Infection
- Bowel obstruction
- Bowel perforation
How do you insert a bowel management system?
- Nonsterile gloves
- Gloves, gown, goggles
- Water for injection – 10ml amps x 5 (need 45ml)
- Dressing pack
- Water-soluble lubricant
- Bowel management system
- Underpads
- Skin-cleansing solution
- Review the patient’s history for possible contraindications
- Evaluate consistency of faecal contents – must be liquid to semi-liquid to flow through the BMS
- Evaluate the patient’s need for analgesia or sedation
- Explain procedure to patient/family when possible
- Wear appropriate PPE
- Position patient in a side-lying position with upper leg flexed
- Clean perineal area with a no-rinse, pH-balanced cleansing solution and trim hair as required
- Perform a manual digital rectal examination to ensure there is no faecal impaction
- Remove anything else from the rectum, such as temperature probes
- Open the BMS kit and connect the pieces according to the manufacturer’s instructions
- Apply water-soluble lubricant to the distal end of the BMS
- With slow, gentle pressure, advance the balloon through the anal sphincter
- Inflate the BMS balloon with water or normal saline solution per instruction guidelines
- Gently pull the BMS back to ensure the balloon is in the rectum and positioned against the rectal floor
- See ‘Management’ section
- Change collection bag as needed
- Inspect every two hours:
- Check patient is not experiencing pain
- Confirm catheter not occluded due to twisting or obstruction
- Ensure no column of faeces or irrigant in catheter – milk into collection bag if present
- Check skin integrity and perianal region for leakage (Small amounts of moisture or seepage around the catheter is anticipated)
- Initiate an appropriate institutional skin care protocol:
- Keep skin clean, dry
- Protected with a moisture barrier product
- If the catheter becomes blocked with faeces, it can be flushed with water:
- Use BLUE irrigation port only, do not use white inflation port (marked “≤45ml”)
- If due to solid stool, use of the device should be discontinued
- Discontinue use once bowel control, consistency and frequency of stool begin to return to normal