RESOURCES
OBJECTIVES & QUESTIONS
Overview
What are the indications for lung resection surgery?
Malignant Conditions
- Non-Small Cell Lung Cancer:
- Those well enough and where curative surgery is possible
- May be combined with extrapleural or en-bloc chest wall resection
- Small Cell Lung Cancer:
- Early-stage disease (T1–2a, N0, M0)
Non-Malignant Conditions
- Large lung bullae
- Infectious disorders:
- Lung abscess
- Tuberculosis
- Trauma
- Congenital disorders:
- A-V fistula
- Sequestrated lobe
- Lobar emphysema
What are the different forms of lung resection surgery?
Wedge Resection
- Surgical removal of a small wedge shaped portion of the lung containing malignant tissue and a rim of healthy tissue surrounding
- Performed to remove small tumours or for diagnosis
- Can be performed when there is a danger of decreased pulmonary function if a lobectomy is performed
- Can be performed by VATS or open thoracotomy
Segment Resection
- Surgical removal of a bronchopulmonary segment along with segmental artery and vein
- Removes a larger portion of the lung than a wedge resection but less tissue than a lobectomy
- Now rarely performed
Lobectomy
- Surgical removal of any of the five lobes
- Right middle and lower are often removed together due to shared lymphatic drainage
- Can be performed by VATS or anterolateral / posterolateral thoracotomy
Pneumonectomy
- Surgical removal of the entire ling
- Radical pneumonectomy include excision of mediastinal glands and dissection of chest wall or pericardium
- Incision is usually posterior lateral thoracotomy
How can lung resection surgery be performed?
Approach
Description
UK Frequency
Open Thoracotomy
- Uses a large single incision (10-15cm) and rib spreading to gain entry to the chest
- Provides good vision and access to the lungs and mediastinum
- Forcible spreading of the ribs to permit the surgeons hands to enter results in great surgical access trauma and associated morbidity
- Significant risk of rib fractures and costovertebral joint damage
43.2%
Video-Assisted Minimal Approach (VATS)
- Uses a main incision (4-6cm), usually with multiple additional incisions, though single port entry is practiced
- Compared to open thoracotomy associated with significantly
- less postoperative pain, less intraoperative blood loss, shorter hospital stays and improved postoperative quality of life
- May offer more limited ability to perform extensive lymph node dissection though 5 years survival outcomes are non-inferior to open surgery
55.8
(10.6% conversion from open)
(10.6% conversion from open)
Robotic-Assisted Minimal Approach (RATS)
- Uses 3-4 small incisions to access the chest with robotic instruments
- Offers the theoretical advantage of 3-dimensional vision and instruments with 360-degree dexterity allowing increased ability to perform complicated proceduresAt present has comparable outcomes to VATS
55.8
(10.6% conversion from open)
(10.6% conversion from open)
What are the outcomes of lung resection surgery?
Mortality varies according to the degree of lung resection performed:
- Pneumonectomy: 4.5% 30-day mortality
- Lobectomy 1.7% 30-day mortality
Patient Selection
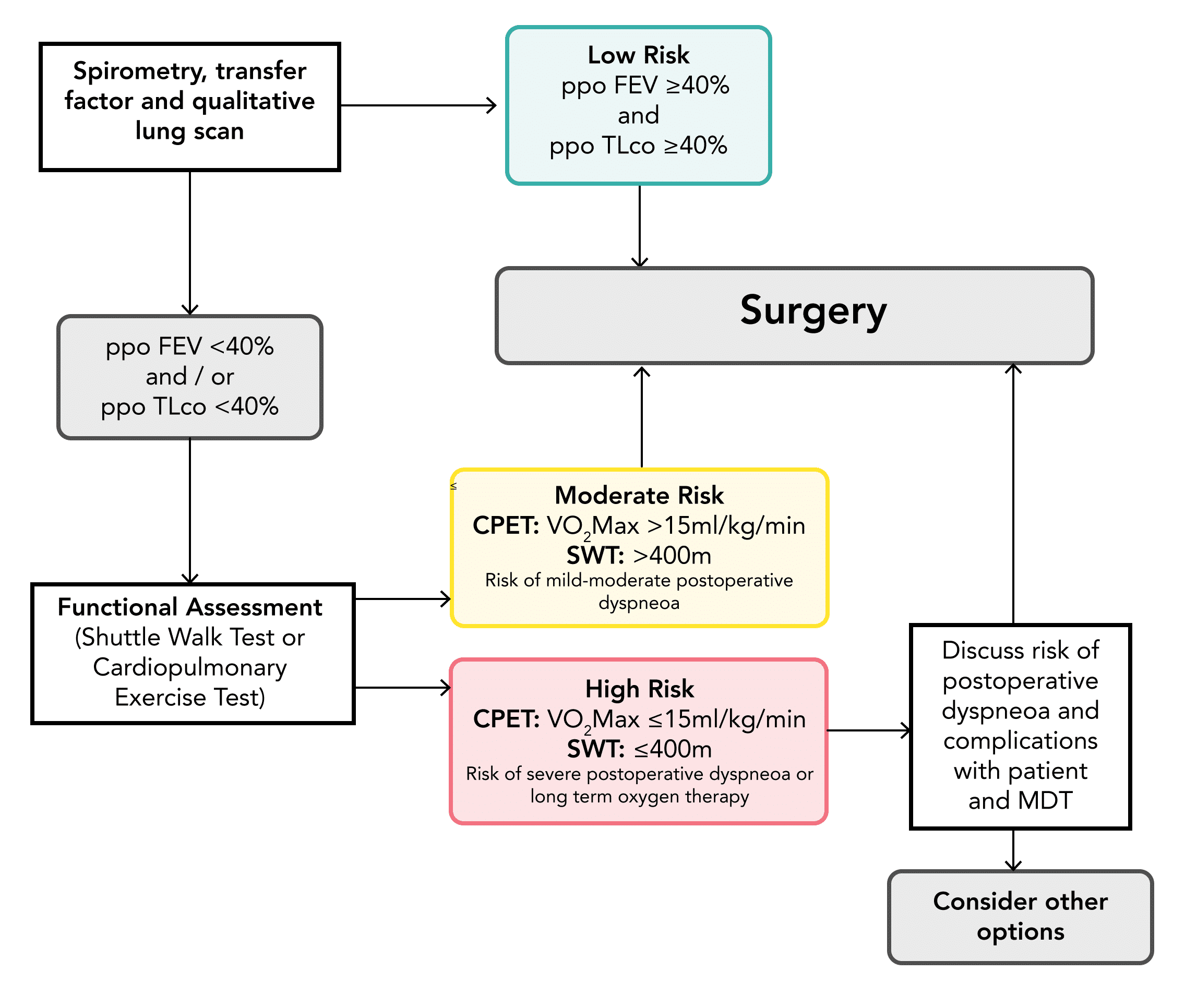
How do you assess fitness for lung resection?
- BTS recommends a tripartite risk assessment model when assessing fitness for lung resection surgery including:
- Risk of operative mortality
- Risk of perioperative myocardial events
- Risk of postoperative dyspnoea
- These can be used to discuss individual risks with the patient and MDT
How is cardiovascular risk assessed?
- BTS guidance suggests the use of the ACC/ AHA risk stratification tool
- Necessitates careful history, physical examination and resting ECG
- All patients with an audible murmur or unexplained dyspnoea should have an echocardiogram
- Patients identified as having an active cardiac condition should be referred for evaluation and optimisation by a cardiologist
What is the thoracascore?
- Thoracoscore is a global risk score used for estimating perioperative death in thoracic surgery
- Uses nine variables (age, sex, ASA score, performance status, dyspnoea score, priority of surgery, extent of surgery, malignant diagnosis and a comorbidity score)
How are tests of pulmonary function used to help determine suitability for lung resection surgery?
- Important in determining risk of:
- Operative mortality
- Postoperative complications
- Postoperative dyspnoea and unacceptable quality of life
- Assessment includes the use:
- Routine lung function tests:
- Spirometry values (FEV1 / FVC)
- Diffusing capacity for carbon monoxide (TLCO)
- Calculated postoperative predicted values using ventilation/perfusion scans or CT evaluation
- Functional assessments (CPET or shuttle walk test)
- Routine lung function tests:
- In changes from previous guidance, specific cut-offs are no longer recommended but used to risk-stratify patients for shared decision making
Which values of pulmonary function are used to determine risk associated with lung resection surgery?
What do the different pulmonary function tests measure?
See section: Pulmonary Function Tests (PFTs)
How is post-resection lung function estimated?
- Postoperative lung function is estimated by the method of ‘segment counting’
- The total number of segments in a normal lung is 19:
- The number of functioning segments preoperatively are calculated:
- Obstructed segments (O) are measured by imaging
- Subtracted from 19 to obtain the number of functioning segments (T)
- The number of segments remaining postoperatively (R) can then be determined
T = 19 - O
R = T - \text{Functioning Segments to be Resected}
- The predicted postoperative (ppo) lung function is then estimated by:
{\text{ppoValue}} = \frac{\text{Preoperative Value}}{T} \times R
How has guidance on selection changed?
- Previous guidelines (2001) advocated a 40% lower limit of ppo FEV1 and TLCO as a cut-off for surgery
- However, evidence has since shown a poor correlation between these values and outcomes:
- Actual postoperative FEV1 and TLCO values are often higher than those predicted using the method of segment counting
- A lower cut-off point (FEV1 and TLCO of 30%) has shown acceptable perioperative mortality
- This has led to recommendations for individually tailored decisions considering the risk of postoperative dyspnoea and impaired quality of life rather than a firm cut-off
Anaesthetic Summary
- Concerns & Goals
- Preoperative Management
- Airway & Induction
- Intraoperative Management
- Postoperative Management
Goals
- Lung isolation to provide optimal surgical field
- Minimisation of acute lung injury during one-lung ventilation
- Safe positioning and careful management of pressure points
- Multimodal analgesia to facilitate postoperative breathing and physiotherapy
- Restrictive fluid therapy and support of haemodynamics
History & Examination
- Full anaesthetic, medical and surgical history paying particular attention to cardiac and respiratory function
- Assessment of smoking history
- Assessment of weight loss and cachexia
- Cardiovascular and respiratory system examination
Investigations
- Laboratory investigations:
- Routine bloods including FBC and U&Es
- Two group and save samples – potential for blood loss from major vessels
- ABG
- Clinical investigations:
- Pulmonary function tests: Spirometry, diffusion capacity (DLCO), predicted postoperative values
- Functional tests: cardiopulmonary exercise testing (CPET), shuttle walk
- ECG – assess cardiac risk
- Imaging investigations:
- CXR
- CT scan
Risk Assessment
- Risk of operative mortality: Thoracoscore
- Risk of perioperative myocardial events: AHA risk stratification +/- cardiology review
- Risk of postoperative dyspnoea: Lung function tests +/- functional tests
Optimisation
- Smoking cessation
- Preoperative physiotherapy
Technique
- Performed under general anaesthesia
Airway Management
- Usually requires lung isolation with either:
- Double lumen tube (most surgeries performed on L sided tube unless chance of left-sided pneumonectomy in which case R sided tube necessitated
- Single lumen tube and bronchial blocker
- Wedge resection can be performed in selected circumstances with spontaneously breathing patient using a supraglottic airway device
Induction & Maintenance
- Volatiles or TIVA used for maintenance
- If volatiles used, MAC >1 can blunt hypoxic pulmonary vasoconstriction
Monitoring
- Lines usually placed on site of surgery where possible to allow easier access
- Ensure wide-bore peripheral access
- Arterial line usually used for blood pressure monitoring and arterial sampling intraoperatively
- Central line may be recommended on a case by case basis for vasopressor infusions given goal of limited fluid therapy, particularly for larger resections such as pneumonectomy
- Catheter and temperature probe essential
Positioning
- Left or right decubitus position with a table break
- Requires fastidious checking of eye protection, pressure points, and neck position
- Tube position should be rechecked with bronchoscopy after positioning
- Compressions stockings and intermittent pneumatic calf compression devices should be used for DVT prophylaxis
Conduct
- Rigid bronchoscope may be performed prior to pneumonectomy
- Requires isolation and one-lung ventilation for surgical access
- Ventilation should be performed to minimise the risk of lung injury:
- Low tidal volumes based on ideal body weight
- Relatively high PEEP
- Low driving pressures
- Avoidance of hyperoxia
Fluids & Haemodynamics
- Fluids should be restricted whilst avoiding hypovolaemia:
- Excess fluid independent risk factor for postoperative pulmonary oedema
- No clear evidence for benefits of goal directed fluid therapy in lung resection surgery
- In the event of hypotension:
- Haemorrhage must be excluded
- Hypotension secondary to epidural infusion should be treated with vasoactive drugs
Analgesia
- Regional anaesthesia useful for intraoperative and postoperative analgesia:
- Single shot:
- Paravertebral block (anaesthetist or surgeon)
- Intercostal blocks
- Erector spinae plane block
- Serratus anterior block
- Retrolaminar block
- Intrapleural analgesia (via drain)
- Continuous:
- Paravertebral infusion
- Epidural infusion
Intrapleural Infusion
- Single shot:
Location & Review
- Traditionally managed in a high dependency environment
- Immediate management on specialist thoracic ward increasingly recognised as safe for low-risk patients
Monitoring & Investigations
- Close monitoring required to allow early recognition of complications
Supportive Care
- Fluids should be restricted whilst avoiding hypovolaemia:
- Excess fluid independent risk factor for post-operative pulmonary oedema
- Fluid balance within the first 24 h should not exceed 20 ml/kg
- Fluid rate often limited to previous hour’s urine output plus 20 ml in the immediate postoperative period
- Ongoing analgesia to allow effective cough and secretion clearance:
- Opioid PCA
- Epidural or paravertebral catheters
- Adjunctive analgesics
- Early and intensive physiotherapy to promote secretion clearance and prevent atelectasis
Management Considerations
What are the key principles in the postoperative care of the patient undergoing lung resection surgery?
- Pain management
- Fluid and electrolyte management
- Physiotherapy and mobilisation
- Safe management and timely removal of chest drains
- Recognition and management of complications
How should pain be managed following lung resection surgery?
- A multimodal approach to analgesia is usually taken
- Opioids remain the mainstay of analgesia usually via PCA
- Often combined with ongoing regional analgesia
What are the options for ongoing regional anaesthesia following postoperative lung-resection surgery?
Epidural Infusion
- Thoracic epidural traditionally used with catheter placed in the midpoint of the dermatomal distribution of the skin incision
- Associated with comparable analgesia to paravertebral block postoperatively
- but significantly more hypotension and urinary retention
- May also reduce the effectiveness of coughing, especially in patients who already have a low FEV1
Paravertebral Infusion
- Increasingly popular option for postoperative analgesia
- Offers the advantage of producing unilateral analgesia and limiting sympathetic block
- Shown to be as effective as thoracic epidural in providing postoperative analgesia with fewer complications
- Can be performed preoperatively by the It can be done by the anaesthetist or under direct vision by the surgeon before closure
Intrapleural Infusion
- Produces a multi-level intercostal block
- However, analgesia is extremely dependent on patient position and infusion volume with significant volumes drained out if chest drains are in situ
- Not found to be reliable in clinical practice and rarely used on a routine basis
How should fluid status be managed following lung resection surgery?
- Judicious approach to fluid management postoperatively generally used to prevent respiratory complications
- Suggested limits for fluid therapy include:
- Maintenance fluids at 1–2 ml/kg/h in the intra- and postoperative period
- A positive fluid balance of 1.5L should not be exceeded in the postoperative period
- If hypoperfusion occurs with threshold limits exceeded, inotropic/vasopressor support should be considered
What are the aims of postoperative physiotherapy following lung resection surgery?
- Clear secretions from remaining lung
- Retain full expansion of remaining lung
- Prevent circulatory complications
- Regain arm and spinal movements
- Maintain good posture
- Restore exercise tolerance
Complications
What are the complications that can occur following lung resection surgery?
Pulmonary
- Pulmonary oedema (9%)
- Post-pneumonectomy syndrome
- Orthodeoxia–platypnoea syndrome
- Lobar torsion (<0.5%)
- Pneumonia
- Atelectasis
- Haemorrhage
- Chronic respiratory failure
Pleural
- Prolonged air leak and persistent pleural space
- Bronchopleural fistula
- Empyema
- Chylothorax
Cardiovascular
- Arrhythmias (AF most common)
- Thromboembolic disease
Other
- Wound infection
- Phrenic nerve injury
- Recurrent laryngeal nerve injury
- Chronic pain
- Death (2%)
What are the risk factors for developing post-operative complications after lung resection surgery?
Patient Factors
- Preoperative PFTs:
- FEV1 <60%
- ppo-FEV1 <30%
- ppo-DLCO <30%
- Age ≥75 years
- BMI ≥30 kg/m2
- Current smoking status
- ASA 3-5
- Disease factors:
- Anaemia:
- COPD
- Liver dysfunction
Procedural Factors
- Major procedure:
- Pneumonectomy
- Extended resection
- Diaphragm or mediastinal resection
- Right sided procedure
- Emergency procedure
- Low level of operator or surgical expertise
- Intraoperative complication
What is post-lung resection pulmonary oedema and how common is it?
- Post-lung resection pulmonary oedema is the occurrence of post-operative pulmonary oedema in the absence of left ventricular dysfunction or infection
- Oedema can occur in either lung though classically affects the contralateral lung
- It is associated with the degree of lung resection with pneumonectomy carrying the highest risk
- The overall incidence is reported as 5.1%
- It is a serious complication associated with a mortality of up to 50%
Why does pulmonary oedema occur after lung resection surgery?
- Post-lung resection pulmonary oedema is non-cardiogenic in origin
- Characterised by increased permeability, oedema and diffuse alveolar damage.
- Mechanisms behind the development are not clearly understand
- Factors believed to contribute include:
- Increase blood perfusion volume through remaining lung
- Intraoperative fluid overload
- Barotrauma / volutrauma from intraoperative mechanical ventilation
- Oxygen toxicity from high intraoperative oxygen concentrations
- Reperfusion injury
- Mediastinal lymphatic interruption
What is post-pneumonectomy syndrome and how does it present?
- A rare postoperative complication caused by excessive mediastinal shift
- Results in impairment of structures close to the mediastinum particularly bronchial compression:
- After right pneumonectomy (more common): Left main bronchus compressed between aortic arch and pulmonary artery
- After left pneumonectomy: Right main bronchus compressed between the pulmonary artery and thoracic spine
- Clinical features include:
- Stridor
- Dyspneoa on exertion
- Recurrent airway infections
- Onset is usually gradual but may be more acute in younger patients
- Definitive management involves surgical repositioning of the mediastinum using a prosthesis
What is orthodeoxia–platypnoea syndrome and how does it present?
- A very rare condition of positional dyspnoea and hypoxemia that can occur following lung resection
- Symptoms occur when the patient is upright and resolve with recumbency
- Exact cause is unclear but thought to be most commonly due to intracardiac shunting
- Altered anatomic relationships following pneumonectomy cause preferential flow from the vena cava through an atrial septal defect or patent foramen ovale towards the left atrium in certain positions
What is lobar torsion and how does it present?
- A very rare complication of lung resection surgery involving rotation of a pulmonary lobe around the hilar pedicle:
- Most commonly involves the right middle lobe following resection of the upper or lower lobe
- Rare reports of involvement of other lobes
- Results in bronchovascular compromise and airway obstruction
- Clinical features include:
- Fever and tachycardia
- Haemoptysis
- Chest pain
- Hypoxia
- Radiographic consolidation
What is a bronchopleural fistula?
See section: Bronchopleural Fistula