RESOURCES
Review Articles
- Pierre, BJA Ed (2013); Nausea and Vomiting After Surgery
- Denholm, Anaes Int Care (2018); Physiology and pharmacology of nausea and vomiting
- Pleuvry, Anaes Int Care (2015); Physiology and pharmacology of nausea and vomiting
- Zhong, Int J Mol Sci (2021); Mechanisms of Nausea and Vomiting: Current Knowledge and Recent Advances in Intracellular Emetic Signaling Systems SI Units, Force, Mass and Acceleration
OBJECTIVES & QUESTIONS
Overview & Definitions
What is postoperative nausea & vomiting (PONV)?
Nausea, retching, or vomiting occurring in the recovery period or the immediate 24 hours postoperatively
How common is PONV?
- Incidence remains high despite widespread use of anti-emetics:
-
- Vomiting: 30%
- Nausea: 50%
- Nausea & vomiting in high-risk groups: 80%
What are the potential adverse consequences of PONV?
- Leads to patient dissatisfaction with anaesthesia (most common cause)
- Severe cases can lead to:
- Increased length of hospital stay / delayed discharge
- Aspiration pneumonia
- Dehydration
- Metabolic alkalosis
- Electrolyte imbalance
- Increased bleeding
- Suture dehiscence
- Incisional hernias
- Oesophageal rupture
Physiology
See Section: Physiology of Nausea & Vomiting
Risk Factors & Prediction
What are the risk factors for developing PONV?
Patient Factors
- Female gender (x3 risk - biggest risk factor)
- Younger age
- Non-smoker
- History of PONV previously
- History of Motion sickness
- Preoperative anxiety
- Disease states:
- Uraemia
- Intestinal obstruction
- Hypoglycaemia
- Hypoxia
Anaesthetic Factors
- Use of specific drugs:
- Inhalational agents (2x risk, dose dependent)
- Nitrous oxide (1.4x risk, likely due to GIT / middle ear cavity distension)
- Opioids (note untreated pain is also emetogenic)
- Sympathomimetics
- Etomidate, ketamine, methohexitone (compared with propofol and thiopentone)
- Neostigmine (recent work suggests that this is not associated with PONV)
- Prolonged anaesthesia
- Spinal anaesthesia (blocks above T5)
- Intraoperative dehydration
- Inexperienced bag and mask ventilation (gastric dilatation)
Surgical Factors
- Specific surgery types:
- Abdominal surgery
- Laparoscopic surgery
- Intracranial surgery
- Middle ear surgery
- Squint surgery (highest incidence of PONV in children)
- Gynaecological
- Head and neck surgery - especially tonsillectomy and adenoidectomy
- Other surgical factors:
- Prolonged surgery
- Painful surgery
Which scoring systems can be used to predict the likelihood of PONV?
Adults
- Apfel score
- Koivuranta score
Children
- POVOC (postoperative vomiting in children) score
What is the Apfel score and how can it be used to predict the likelihood of PONV?
Characteristics
Points
Female sex
1
History of motion sickness or postoperative nausea and vomiting
1
Non-smoker
1
Postoperative opioid treatment is planned
1
Sum
0-4
Score
Probability of postoperative nausea and vomiting (%)
0
10
1
20
2
40
3
60
4
80
What is the POVOC score and how can it be used to predict the likelihood of PONV in children?
Characteristics
Points
Duration of sugery >30 mins
1
Age ≥3
1
Strabismus surgery
1
History of PONV in a relative
1
Sum
0-4
Score
Probability of postoperative nausea and vomiting (%)
0
9
1
10
2
30
3
55
4
70
Prevention
What strategies can be used to prevent PONV?
Pharmacological
- Anti-emetic drugs:
- Serotonin (5-HT3 receptor) antagonists
- Corticosteroids
- Butyrephenone
- Neurokinin (NK1) antagonists
- Anticholinergics
- Dopamine antagonists
- Propofol
- Modification of anaesthetic technique:
- TIVA
- Avoidance of volatiles and nitrous oxide
- Avoidance of neostigmine reversal
- Minimization of opioid use
Non-Pharmacological
- Preoperative and intraoperative fluid therapy
- Regional techniques (opioid sparing)
- Acupuncture
- Minimization of anaesthesia & surgery length
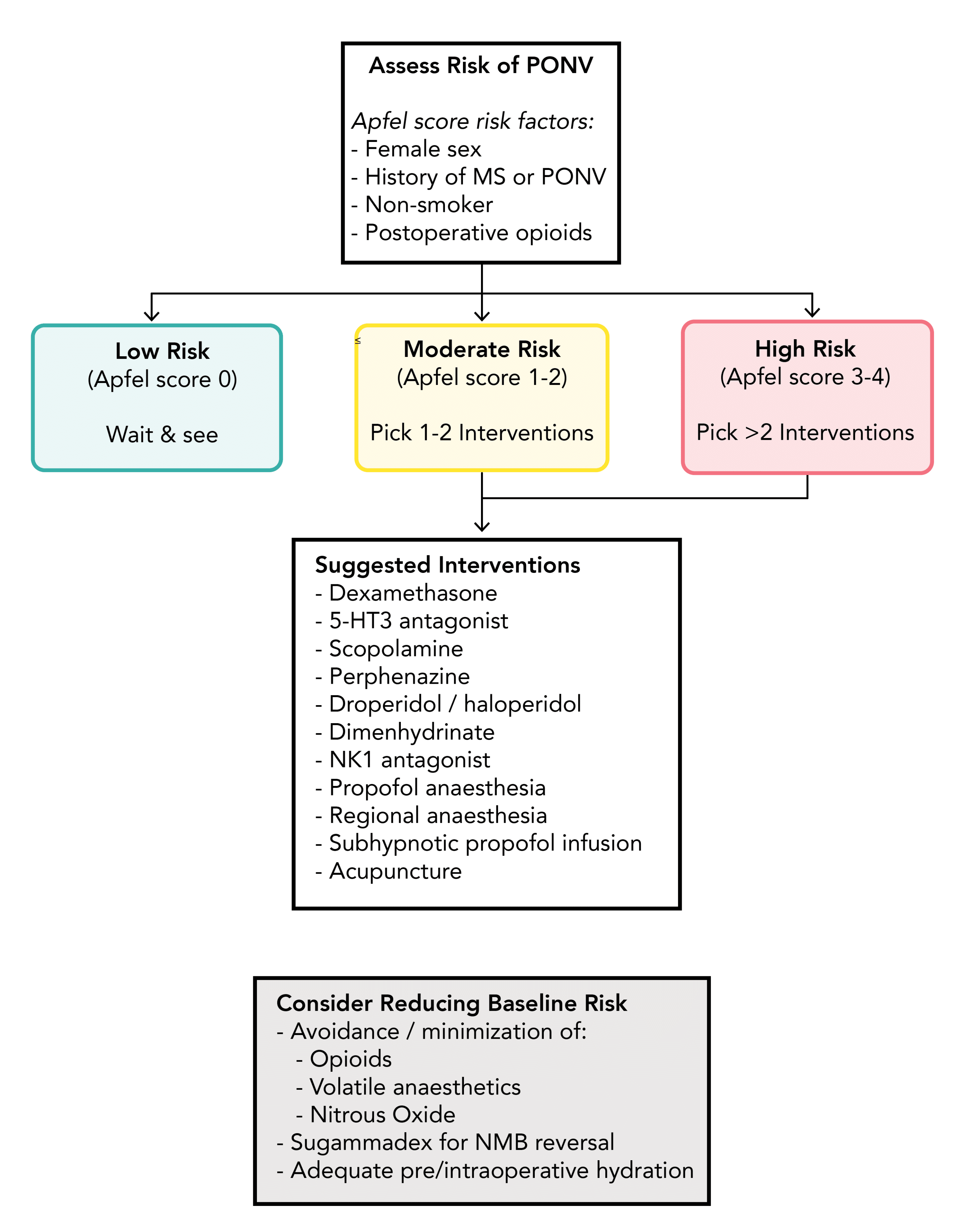
What is the suggested way for determining which strategies to use for preventing PONV?
Which are the most effective antiemetic drugs for preventing PONV?
Drug
Risk Ratio for PONV
Risk of Adverse Events
Fosaprepitant
0.06
N/A
Casopitant
0.16
Very low
Aprepitant
0.26
Very low
Ramosetron
0.44
Very low
Granisetron
0.45
Moderate
Dexamethasone
0.51
Low
Tropisetron
0.52
Low
Ondansetron
0.55
Low
Dolasetron
0.56
Very low
Droperidol
0.61
Low
Scopolamine
0.61
High
Haloperidol
0.61
N/A
Metoclopramide
0.73
Low
Cyclizine
0.83
N/A
Which are the most effective antiemetic drugs for preventing PONV?
Group
Drug
Dose
Timing
Adverse Effect
Serotonin (5-HT3 receptor) anatagonists
Ondansetron
4-8mg IV
End of surgery
Headaches, constipation, raised liver enzymes
Serotonin (5-HT3 receptor) anatagonists
Granisetron
1mg IV
End of surgery
Headaches, constipation, raised liver enzymes
Serotonin (5-HT3 receptor) anatagonists
Tropistron
2mg IV
End of surgery
Headaches, constipation, raised liver enzymes
Corticosteroids
Dexamethasone
4-10mg IV
After Induction of Anaesthesia
Increased blood glucose level, hyper/hypotension
Neurokinin (NK-1 receptor) antagonists
Aprepitant
40-80mg PO
Before Induction of Anaesthesia
Headaches, constipation, fatigue
Neurokinin (NK-1 receptor) antagonists
Fosaprepitant
150mg IV
Before Induction of Anaesthesia
Headaches, constipation, fatigue
Neurokinin (NK-1 receptor) antagonists
Casopitant
150mg PO
Before Induction of Anaesthesia
Headaches, constipation, fatigue
Anticholinergics
Scopolamine (Hyoscine)
Transdermal patch
Before Induction of Anaesthesia
Dizziness, dry mouth, visual disturbance
Dopamine Antagonists & Butyrophenones
Metoclopramide
10-25mg IV
After Induction of Anaesthesia
Sedation, hypotension (fast injection)
Dopamine Antagonists & Butyrophenones
Droperidol
0.625-1/25mg IV
After Induction of Anaesthesia
Sedation, hypotension (fast injection)
Dopamine Antagonists & Butyrophenones
Haloperidol
1-2mg IV
After Induction of Anaesthesia
Sedation, hypotension (fast injection)
Anthistamine
Dimenhydrinate
25-50mg IV
After Induction of Anaesthesia
Which are the most effective antiemetic drugs for preventing PONV?
- Adequate hydration is a proven effective strategy for reducing the risk of PONV:
- Minimisation of perioperative fasting time
- Perioperative use of IV fluid to maintain euvolemia
- Intraoperative supplemental crystalloid bolus (10–30 mL/kg)
Management
How should the pharmacological management of PONV be approached postoperatively?
- Administer an antiemetic from a different pharmacologic class from the prophylactic drugs initially given
- If no prophylaxis is given, first-line is recommended as a low-dose 5-HT3 antagonist
- Other options include dexamethasone or promethazine / cyclizine
- Haloperidol should only be used for adults
- Droperidol should only be in children if other options have failed
- Propofol 20mg may be considered as a useful rescue therapy
- Drugs should only be readministered if > 6 hours postoperative:
- Dexamethasone and scopolamine should not be readministered