RESOURCES
Guidelines
Review Articles
- Papavramidis, J Emerg Trauma Shock (2011); Abdominal compartment syndrome – Intra-abdominal hypertension: Defining, diagnosing, and managing
- Cheatham, S Journal Trauma, Resus & Em Med (2009); Review Article – Abdominal Compartment Syndrome – Pathophysiology and Definitions
- Bailey, Critical Care (2000); Abdominal compartment syndrome
OBJECTIVES & QUESTIONS
Introduction & Definition
What is normal intra-abdominal pressure (IAP)?
- IAP is approximately 5–7 mmHg in critically ill adults
- It is not static and varies with respiration
What is Intra-abdominal hypertension (IAH) and how is it graded?
IAH is defined by the World Society of Abdominal Compartment Syndrome as:
A sustained or repeated pathological elevation in IAP >12 mmHg
It is graded according according to pressure:
What is abdominal compartment syndrome?
ACS is defined by the World Society of Abdominal Compartment Syndrome as:
A sustained IAP >20 mmHg that is associated with new organ dysfunction/failure
Epidemiology, Clinical Course & Prognosis
How common are IAH and ACS?
- Commonly seen in ventilated critically ill patients
- A large prospective study of at-risk critical care patients found an incidence of:
- 33% of patients developing intrabdominal hypertension
- 3.6% of patients developing abdominal compartment syndrome
What is the course and prognosis of abdominal compartment syndrome?
- Severity of organ failure related to the duration of intra-abdominal hypertension
- Abdominal compartment syndrome carries a poor prognosis:
- Without treatment the mortality is 100%
- Studies have shown mortality of 35-50% despite treatment
Aetiology
What are primary and secondary ACS?
- Due to a condition associated with injury or disease in the abdominopelvic region
- Frequently requires early surgical or interventional radiological intervention
- Due to a conditions that do not originate from the abdominopelvic region
What are the risk factors for and causes of abdominal compartment syndrome?
Decreased Abdominal Wall Compliance
- Abdominal surgery
- Prone positioning
- Major trauma
- Major burns
Increased Intra-luminal Contents
- Gastroparesis / gastric distension
- Ileus / colonic pseudo-obstruction
- Volvulus
Increased Intra-luminal Contents
- Acute pancreatitis
- Haemoperitoneum / pneumoperitoneum / intrabdominal fluid collection
- Intra-abdominal infection / abscess
- Liver dysfunction with ascites
- Intra-abdominal /retroperitoneal tumour
- Peritoneal dialysis
Capillary Leak / Fluid Resuscitation
- Sepsis
- Acidosis
- Hypothermia
- Increased APACHE score
- Massive fluid resuscitation
- Polytransfusion
- Major trauma / burns
Capillary Leak / Fluid Resuscitation
- Obesity
- High PEEP
- Pneumonia
- Coagulopathy
Pathophysiology
How does raised intra-abdominal pressure affect other organ systems in abdominal compartment syndrome?
- Diaphragmatic splinting and extrinsic compression of lung tissue
- Leads to:
- Reduced compliance and increased airway pressures
- Increased ventilation/perfusion (V/Q) mismatch
- Basal atelectasis and collapse, hypoxemia and hypercapnia
- Cardiac output reduced due to:
- Decreased venous return due to venous compression
- Increased afterload due to aortic compression
- Increased intra-thoracic pressure due to diaphragmatic splinting may compromise CO further:
- Decreased ventricular compliance and contractility
- Decreased ventricular compliance and contractility
- Raised ICP due to:
- Impaired CSF absorption in the lumbar plexus
- Impaired jugular venous return
- Increased further due to cerebral vasodilatation caused by concomitant hypoxaemia and hypercapnia
- Renal failure due to:
- Reduced renal blood flow
- Increased pressure within the tubules and reducing the filtration gradient
- Compensatory activation of the renin-angiotensin-aldosterone (RAA) worsening the renal insult
- Bowel wall venous obstruction and hypertension due to compression effect resulting in oedema and further reduced compliance
- Bowel ischaemia and bacterial translocation increases the risk of sepsis
- Reduced hepatic artery, vein and portal system flow leading to liver dysfunction
- Biliary stasis due to increased pressure within the biliary tree
Abdominal Pressure Measurement
Who should have intrabdominal pressures (IAP) measured?
- The WSACS has recommended that all critically ill patients with any risk factor for the development of IAH/ACS should have IAP measured
- If pressures are elevated, serial measurements should be performed every 4-6 hours
Which methods can be used to measure intrabdominal pressure?
Pressure measured from the peritoneum:
- At laparoscopy
- Peritoneal pressure transducer
- Peritoneal drain
Pressure measured via:
- Bladder (Reference Standard):
- Foley catheter pressure transducer (Modified Kron method) - Most common
- Foley catheter manometer (Harrahill method)
- T-Doc air charged catheter
- Stomach
- Nasogastric tube pressure transducer
- GastroManometer
- CiMon
- Rectum
- Vagina
- Inferior Vena Cava
Which method is recommended for measuring intrabdominal pressure?
- It is recommended that intravesicular pressure is measured via foley catheter
- The ‘Modified Kron’ method is the most popular method due to its simplicity and low cost:
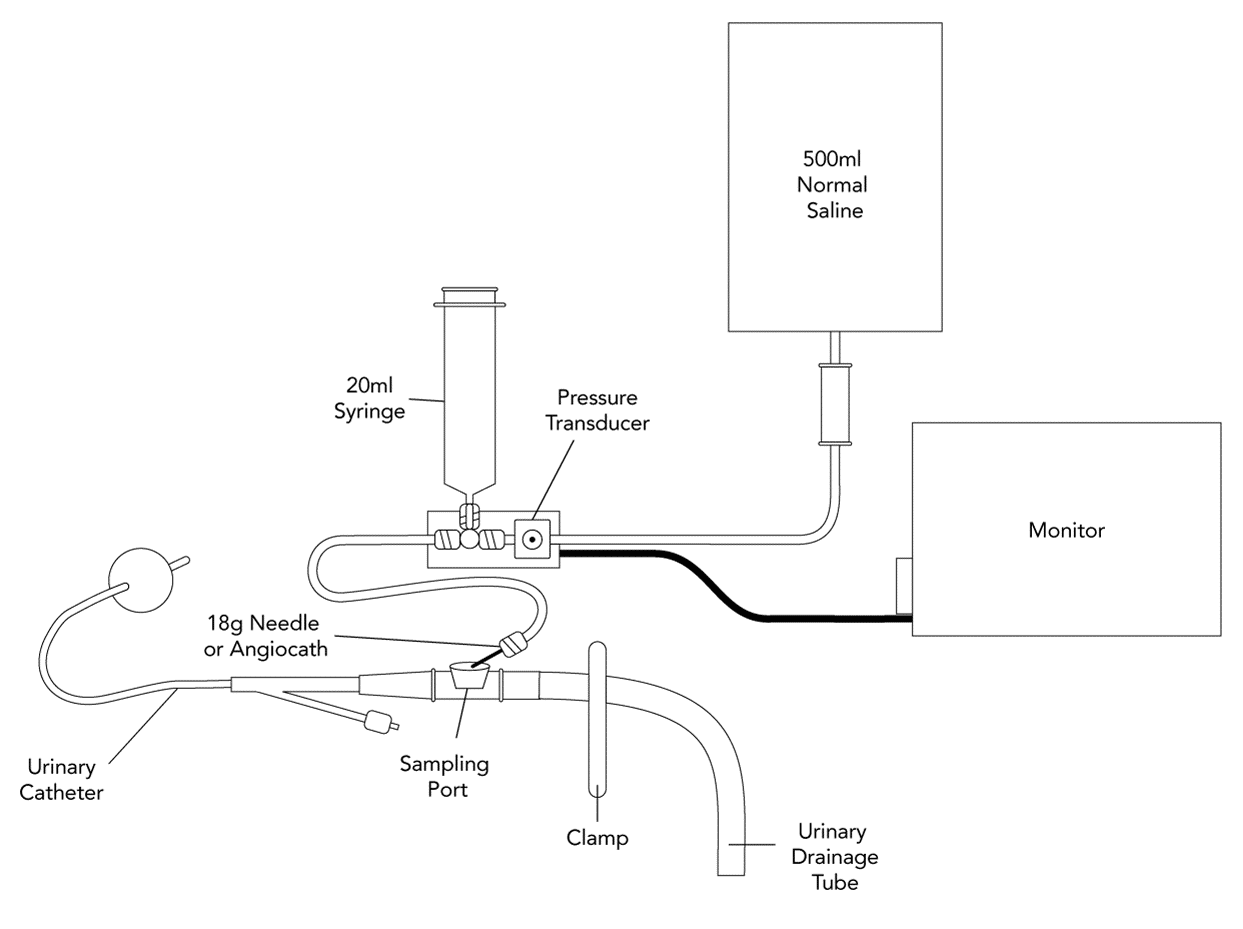
- Wash hands and follow universal antiseptic precautions
- Insert a foley catheter and connect a urinary drainage system
- Using a sterile field and gloves, the drainage tubing is cut (with sterile scissors) 40 cm after the culture aspiration port after disinfection.
- Set up a pressure transducer set:
- Connect to a bag of 500 mL of normal saline and ensure system is flushed
- Connect a 20ml syringe to the 3 way tap
- Select a scale from 0 to 20 or 40 mm Hg on the monitor
- Patient should in the supine position for measurement:
- If not clinically feasible:
- Recognize head elevation will result in a higher pressure
- Ensure all subsequent readings are taken in the same position.
- Adjust the height of the transducers and ensure it is zeroed level with the mid-axillary line
- Clamp the drainage tube to the urine bag
- Connect the needle to the rigid tubing of the pressure transducer
- Insert the needle into the sampling port of the catheter
- Fill the bladder with 1ml/kg (maximum 25mls) of 0.9% sodium chloride using the syringe
- Close the stopcock of the syringe and allow 30 seconds for equilibrium to occur
- Obtain the mean pressure reading upon end-expiration to minimize the effects of pulmonary pressures
- Fluctuations in the pressure waveform should be seen with pulsations in abdominal blood flow.
Management Summary
How do you manage the patient with abdominal compartment syndrome (ACS)?
Key Principles
- Resuscitation and management of underlying condition
- Treatments to improve wall compliance and evacuate intra-abdominal contents
- Optimise tissue perfusion
- ABCDE approach:
- Intubation and ventilation if respiratory distress
- Optimize ventilatory support
- Fluid and vasopressor resuscitation if compromised hemodynamics
- Treat the underlying cause
1. Improve abdominal wall compliance:
- Adequate sedation and analgesia
- Ensure no external constriction e.g. dressings/eschars
- Appropriate positioning:
- Avoid proning/head up>20°
- Consider reverse Trendelenburg positioning
- Neuromuscular blockade
2. Treatments to evacuate intra-luminal content:
- Nasogastric/rectal decompression via aspiration/free drainage of nasogastric/rectal tubes;
- Administration of gastric/colonic prokinetics - caution after surgery
- Reduce enteral nutrition volume
- Enemas
- Colonoscopic decompression
3. Treatments to identify and evacuate intra-abdominal collections:
- Abdominal imaging
- Drainage:
- Percutaneous drainage or paracentesis
- Surgical evacuation
4. Treatments to optimize fluid balance:
- Optimal, not excessive, fluid resuscitation
- Hypertonic solutions and colloids; diuretics to drive negative fluid balance if haemodynamically stable
- Renal replacement therapy
5. Treatments to optimize tissue perfusion to maintain an abdominal perfusion pressure:
- Use goal directed fluid resuscitation
- Vasoactive drugs
If refractory to medical management consider surgical management with abdominal decompression
- Monitor IAP every 4-6 hours if elevated
- The WSACS approach an algorithm with a 4 step approach for each treatment arm
- Treatment arms should be addressed simultaneously and tailored to the individual patient
Supportive Care
What is the abdominal perfusion pressure (APP)?
- APP abdominal perfusion pressure (APP) is the blood pressure perfusing abdominal viscera
- It can be considered the abdominal analogue to cerebral perfusion pressure
- It is calculated using the formula:
Abdominal Perfusion Pressure = Mean Arterial Pressure – Intra-abdominal Pressure
What APP should be targeted during resuscitation in ACS?
- Previously, the WSACS recommended that the APP be maintained above 60mmHg in an attempt to provide adequate visceral perfusion
- Still widely practised but recommendation no longer given due to lack of evidence


