RESOURCES
OBJECTIVES & QUESTIONS
Overview
What is laryngoscopy?
- Describes the visualization or examination of the laryngeal inlet by distraction of the upper airway structures
- It is generally performed to allow:
- Tracheal intubation
- Removal of laryngeal and pharyngeal foreign body or suctioning
- Placing of nasogastric tubes, throat packs and other devices
What types of laryngoscopy can be performed?
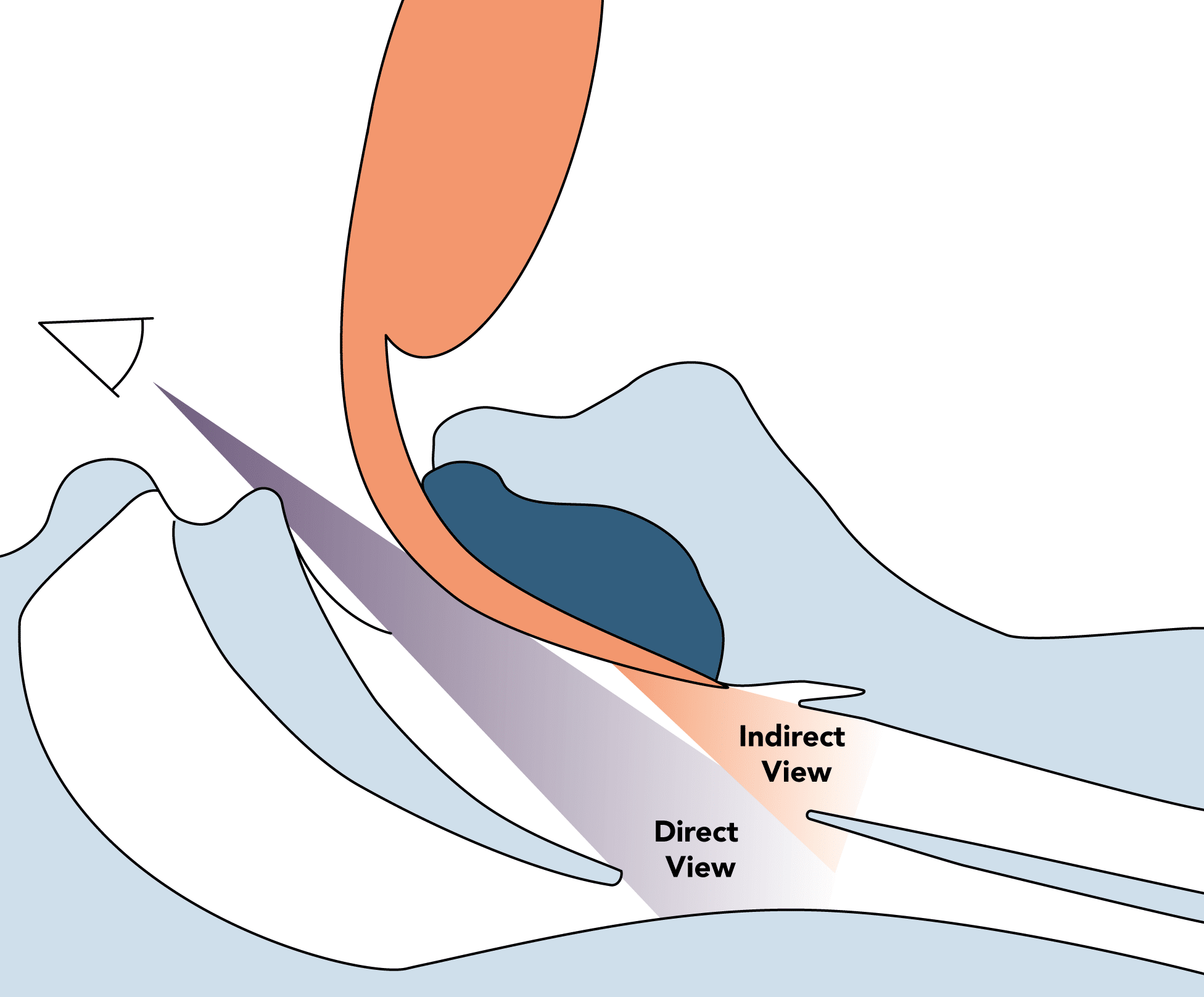
Direct Laryngoscopy
- Visualisation of the laryngeal inlet in direct line of sight
Indirect Laryngoscopy
- Visualisation of the laryngeal inlet with methods other than direct vision through the use of optic, fibreoptic or video systems
How can you classify laryngoscopes?
Direct Laryngoscopes
- Straight Blade
- Curved Blade
Indirect Laryngoscopes
- Rigid Blade
- Integrated channel laryngoscopes
- Video Stylet
Cleaning & Decontamination
What are the infection control concerns with laryngoscopes?
- Well recognised source of cross-contamination:
- High-risk instruments, regularly contaminated with blood
- Have been implicated as possible transmitters of CJD
- Both the handle and blade can become contaminated during use
How can infection concerns be overcome?
- Single-use laryngoscope blades are encouraged:
- Not been shown to be associated with an increased risk of complications
- Use can be economical when sterilisation costs considered
- If reusable laryngoscopes are used:
- Blades should be sterilised by a regulated sterile supply department between uses
- Handles should be disinfected or sterilised between uses
- If video laryngoscopes are used:
- Single-use blades are encouraged
- Decontamination of reusable components must happen after each use in a standardised manner
- Care should be taken to place used scopes in a designated receptacle after use to prevent contamination
Overview
What are the components of a direct laryngoscope?
Typically consists of:
Handle
- Provides an area to grip and storage for the batteries
Light Source
- Illuminates the tip of the blade
Blade
- Displaces the tongue and epiglottis to achieve a view of the laryngeal opening
Blades
What are the components of the laryngoscope blade?
Spatula
(Tongue)
(Tongue)
- The main part of the blade which may be straight or curved
- Passes over the lingual surface of the tongue
Flange
- The portion of the blade that arises from the edge of the spatula
- Used to direct and compress the tongue and other tissue to reveal the cords
- Size and shape varies significantly with different blade designs
Web
- Connects the flange to the spatula
Tip
(Beak)
(Beak)
- Contacts the vallecula to directly or indirectly elevate the epiglottis
- Is usually blunt and thickened to prevent trauma
Base
- Attaches the blade to the handle
- Has a notch to engage with the hinge pin of the handle
What is the difference between straight and curved laryngoscope blades?
Type
Description
Advantages & Disadvantages
Curved Blade
Designed to lift the epiglottis indirectly and provide a view of the laryngeal opening by placing the tip over the epiglottis into the vallecula and exerting pressure on the hypoepiglottic ligament
- Less traumatic
- Less stimulating
- Provides better view in patients with big tongues
Straight Blade
Designed to be placed under the epiglottis and lift it directly to provide a view of the laryngeal opening
- More traumatic
- More stimulating due to contact with epiglottis - can trigger tachycardia and arrythmias
- Provides better view in patients with long, floppy or anterior epiglottis (neonates, infants and children)
What types of curved laryngoscope blade are commonly available?
Macintosh
- The most commonly used blade in the UK
- A gentle curve from the tip to the proximal end
- Large 'reverse-Z' flange designed to sweep the tongue to the left of the mouth
- Light source pierces the blade towards the tip so as not to interfere with the view
McCoy
- A modification of a Macintosh blade
- Has a hinged tip which can be lifted using the lever attached to the handle
- Designed to lift the epiglottis with less force than a standard mackintosh
- Can be useful in achieving a better view than a standard Macintosh blade particularly in cervical spine injury
Robertshaw
- Gently curved over the distal third
- Designed to indirectly lift the epiglottis like a Macintosh blade
- Generally used in infants and children
- Allows binocular vision by removing the lateral flange
Polio
- A modification of the Macintosh blade
- Mounted on the handle at 135° rather than 90°
- Initially used in polio patients ventilated with an iron lung but now occasionally used in conjunction with a stubby handle in patients with large breasts or restricted neck movement
What types of straight laryngoscope blade are commonly available?
Miller
- The most commonly used straight blade in the UK
- The small tongue does not allow a sweep of the tongue but is designed to be directed along the right side of the mouth and re angled once passed the base of tongue
Seward
- Originally designed for use in neonates
- Incorporates a low profile flange
Wisconsin
- Has a flange that expands slightly toward the distal portion of the blade
- Increases the visual field and possibly reduces trauma
Handles
What are the different types of laryngoscope handles available?
Standard
Standard
- Designed for use with adult blades
- Has a hinge pin for the attachment of the blade and a barrel to store batteries and a light
Penlight
Penlight
- Designed for improved balance with paediatric blades
Stubby
Stubby
- Designed to reduce the obstruction caused by large breasts or a barrel chest
Light Sources
What are the features of different light sources available on laryngoscopes?
Standard Light Source
(Colour Coded Black)
(Colour Coded Black)
- Contains a small bulb near the distal end of each blade
- Handle contains the batteries only
- Bulbs can be standard filament or LED
- Filament bulbs can cast small central shadow
- Bulbs generate heat and risk of thermal transmission to patient with standard bulbs (not with LEDs
- Handles are black or silver
Fibreoptic Light Source
(Colour Coded Green)
(Colour Coded Green)
- Contains the bulb and batteries in the handle
- Transmitted to the blade through a fibreoptic column
- Avoids the risk of heat transmission
- Can allow for brighter bulbs to be used
- Disposable blades more economical
- Handles are green or silver with green band
Overview
How do indirect laryngoscopes work?
- Designed to look around the “anatomical corner’’ at the laryngeal inlet
- Do not require optimization of the oral, pharyngeal, and tracheal axes
- Require less force to achieve a view
- Useful in difficult airways where it may be a challenge to get a view of the glottic opening
- Although obtaining a view is often easier can be difficult in passing a tube due to the resultant increased glottic angulation:
- Can be overcome through the use of incorporated channel, stylet or bougie
What are the ways of providing an indirect view of the larynx?
Videolaryngoscopes
Transmits an image to the viewfinder or screen electronically from a distal tip video camera
Optical Laryngoscopes
Transmits a magnified image to the viewfinder via reflection through prisms, mirrors or fibreoptics
How can you classify indirect laryngoscopes?
Non-Guided (Standard Blade or Angulated Blade) Devices
Provide an indirect view of the larynx, but require direction of the TT towards the larynx
- Storz CMAC
- McGrath MAC
- Glidescope
Guided (Channelled) Devices
Provide an indirect view of the larynx and a conduit for passage of the TT
- Airtraq Laryngoscope (Optical)
- Pentax Airway scope
Optical Stylets
Provide an indirect view via a rigid or semi-rigid stylet, with a ‘loaded’ TT for railroading
- Bonfils
- Shikani
What are the advantages and disadvantages of indirect laryngoscopes?
Advantages
- Improved laryngeal visualization
- Improved intubation success
- Greater portability than fibreoptic scopes
- Reduced trauma
- Reduced force required:
- Results in less cervical spine movement
- Less haemodynamic stress
- Easy to learn
- Useful in airway training:
- Allows concurrent view by observer
Disadvantages
- Difficulty in inserting tube despite good view:
- Often Requires bougie or stylet
- Reduced skill in ‘gold standard’ technique of direct laryngoscopy
- Increased cost over standard laryngoscopes
- Large handle can be difficult to insert in pregnant or obese patients
Videolaryngoscopes
What types of videolaryngoscopes are commonly available and what are their features?
Glidescope
- A non-guided videolaryngoscope
- Has a camera on the end of a reusable video baton which is placed inside disposable plastic blades
- A heater at the lens prevents fogging
- Requires the use of a stylets preformed in the shape of the blade
CMAC
- A non-guided videolaryngoscope
- Can be used with single use or reusable blades
- Blades can be either MacIntosh, Miller or angulated "D" style
- Can be used for both direct and indirect laryngoscopy
- Has an integrated white balance and antifogging system
McGrath
- A non-guided videolaryngoscope
- Has a screen mounted on the handle making it compact and portable
- Uses disposable plastic Macintosh blades mounts mounted over a on-disposable camera
- Can be used for both direct and indirect laryngoscopy
- Blades have less curvature than other models
Airtraq
- An optical guided laryngoscope
- Single use disposable device supplied with batteries in situ
- Has an LED light source at the tip with the view provided via prisms and mirrors to an eyepiece
- Incorporates a tube channel to guide the tube ut may make it difficult to feed unless well lubricated
- Comes in paediatric sizes and additional designs for nasal and double lumen intubations
- Attachments are available to mount a camera to the eyepiece