RESOURCES
Review Articles
- Khan, Anaesthesia (1999); Alpha-2 and imidazoline receptor agonists
- Giovannitti, Anesthesia Progress (2015); Alpha-2 Adrenergic Receptor Agonists: A Review of Current Clinical Application
- Maud, Clin Pharmacokinet (2017); Clinical Pharmacokinetics and Pharmacodynamics of Dexmedetomidine
- Jamadharkana, J Anaesth Clin Pharmacol (2010); Clonidine in Adults as a Sedative Agent in the Intensive Care Unit
- Fernandes, Biomed J Sci&Tech Res (2018); Clonidine in Anesthesiology: A Brief Review
- Kaur, Anesthesia: Essays and Researches (2011); Current role of dexmedetomidine in clinical anesthesia and intensive care
- Scott-Warren, BJA Ed (2016); Dexmedetomidine: its use in intensive care medicine and anaesthesia
OBJECTIVES & QUESTIONS
Overview, Mechanisms & Effects
What are alpha-2 agonists?
- A group of centrally acting drugs used primarily for their sedative and analgesic properties
- Produce dose-dependent interactive sedation that resembles natural sleep with minimal respiratory depression compared to traditional sedatives
What are the clinically available alpha-2 agonists?
- Several alpha-2 agonists are available:
- Clonidine
- Dexmedetomidine
- Medetomidine
- Tizanidine
- Guanfacine
- Of these, only clonidine and dexmedetomidine are regularly used in the UK
What are the alpha-2 receptors, and what are their functions?
- Belong to a family of membrane-bound guanine nucleotide-binding protein-coupled receptors
- Consists of three main subtypes with different actions:
- Suppresses neuronal firing reducing the activity of ascending noradrenergic pathways:
- Sedative and anxiolytic effects
- Directly stimulate presynaptic α2A- and α2C-adrenoceptors in the spinal cord, thereby inhibiting the firing of nociceptive neurons
- Analgesic (anti-nociceptive) effect
- Reduces sympathetic outflow (sympatholytic action):
- Reduces sympathetic tone (promotes hypotension)
- Reduces cardiac sympathetic activity (reduces heart rate, cardiac output and myocardial oxygen consumption)
- Reduces renal sympathetic activity (inhibits renin and vasopressin release, promotes diuresis)
- Vasoconstriction
- Unclear clinical effects
- Postulated to have anxiolytic effects
Which receptors do clonidine and dexmedetomidine act on?
- Clonidine and dexmedetomidine are not pure alpha-2 adrenoceptor agonists, but also act at several different receptors
- Specific drug effects depend on the relative selectivity for each receptor type:
- Primarily sedation and anxiolysis
- Reduce sympathetic outflow resulting in hypotension and bradycardia
- Peripheral vasoconstriction & hypertension
- Centrally mediated hypotension
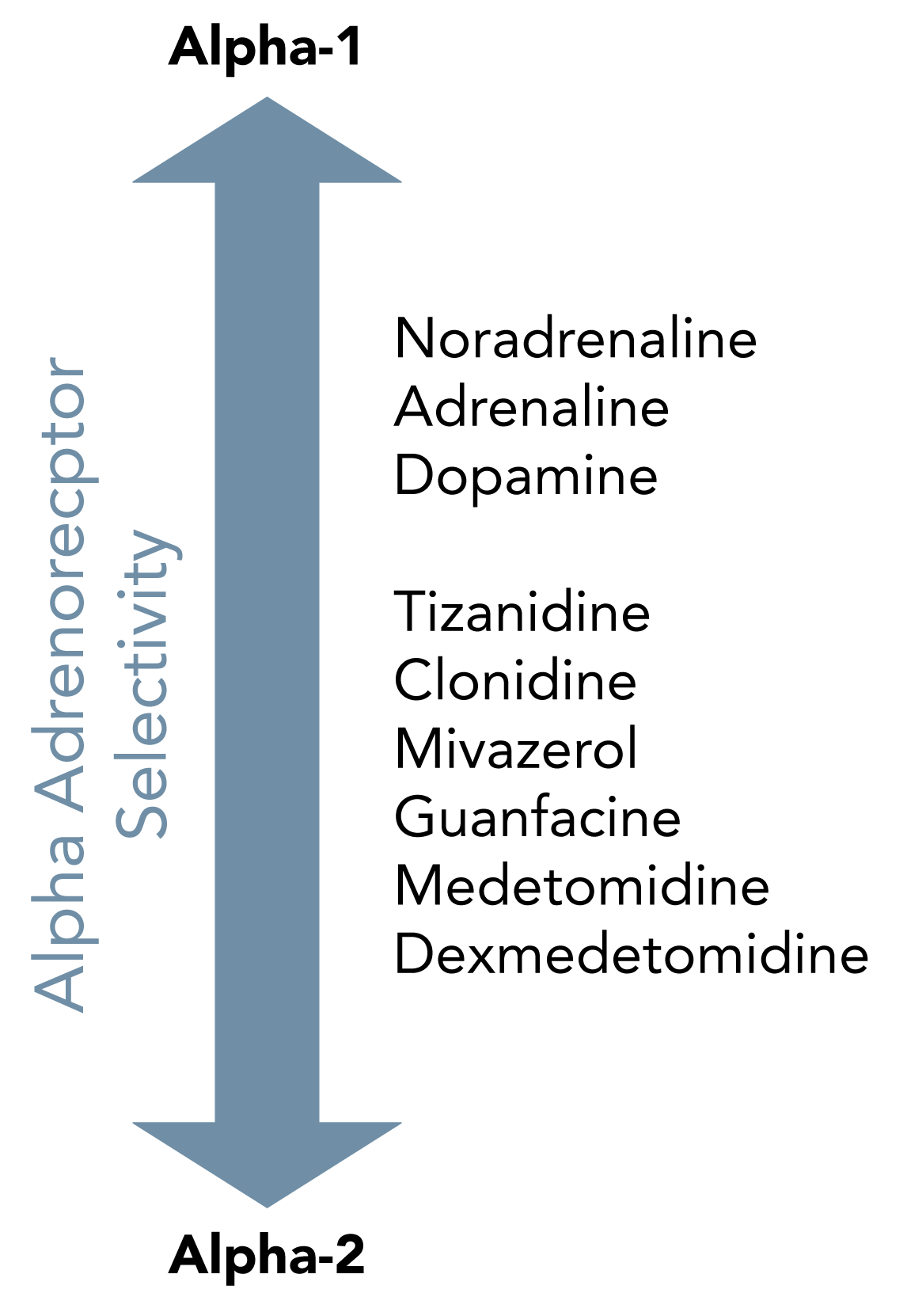
Where do common alpha-2 agonists sit in the spectrum of alpha-1 and alpha-2 agonism?
Comparison
What are the key clinical similarities and differences between clonidine and dexmedetomidine?
- Administered orally, transdermally, or intravenously
- Administered via intravenous infusion only
- Onset of action 10 minutes IV
- Terminal half-life ~7 hours
- 20% bound to plasma proteins
- Volume distribution of 1.7–2.5 L/kg
- 40% hepatically metabolised to inactive metabolites
- 60% excreted renally unchanged
- Accumulates in renal failure
- Onset of action <5 minutes IV
- Half-life 2 hours
- 90% bound to plasma proteins
- Volume distribution of 1.3–2.4 L/kg
- Primarily hepatically metabolised to inactive metabolites
- Does not accumulate in renal failure
- Lesser selectivity for α2-adrenoceptors (α2:α1 ratio 220:1)
- Greater agonism at imidazoline receptors and therefore tends to cause more hypotension
- Greater selectivity for α2-adrenoceptors (α2:α1 ratio 1,620:1) producing more potent sedation
- Lesser action on imidazoline receptors
- Cheap - estimated cost £8/day
- Expensive - estimated cost £100/day
- Used as sedative, analgesic and anaesthetic adjunct
- Availability of oral and transdermal formulations makes it easier to use in non-intensive care settings
- Primarily used as a sedative for procedures or intensive care
- Better suited for intensive care than clonidine due to:
- Increased titratability
- Rapid onset of sedative effect
- Predictable haemodynamic response with less prominent hypotension and bradycardia
- Better pharmacokinetic profile in renal failure
Clinical Essentials
- Alpha-2 agonist with sedative and analgesic effects
- Produces sedation without significant effect on respiratory drive
- Used for multiple indications across anaesthesia, critical care and pain management
- An older drug which has been superseded by dexmedetomidine for some indications
- Alpha-2 agonist with sedative and analgesic effects
- Produces sedation without significant effect on respiratory drive
- Used for multiple indications across anaesthesia, critical care and pain management
- An older drug which has been superseded by dexmedetomidine for some indications
Sedation on critical care
- Sedation of intubated and mechanically ventilated patients as an adjunct to other sedatives
- Treatment of agitated and delirious patients
- Must be weaned gradually
IV/PO: 50-200 mcg QDS
Adjunct to anaesthesia
- Reduces MAC of volatile agents
Adjunct to perioperative analgesia
Adjunct to regional anaesthesia
- Prolongs duration of effect
- Useful in peripheral nerve, epidural, caudal and spinal blocks
Anxiolysis (Premedication)
- May be a useful in both children and adults (though onset is slow)
Antihypertensive
- Medical use is limited by severe rebound hypertension following discontinuation
- May be useful for hypotensive anaesthesia
Alcohol & opiate withdrawal
Postoperative shivering
Migraine prophylaxis
- No definitive contraindications
- Extreme caution should be exercised in patients with:
- Heart block
- Bradycardia
- Hypotension or hypovolaemia
- Severe ventricular dysfunction
- Peripheral vascular disease
- Concomitant use of:
- Beta-blockers (bradycardia)
- Tricyclic antidepressants (counteract effect)
- Digoxin (bradycardia)
- Haloperidol (prolongation of QT interval)
- Sudden withdrawal should be avoided due to the risk of rebound hypertension
- No definitive contraindications
- Extreme caution should be exercised in patients with:
- Heart block
- Bradycardia
- Hypotension or hypovolaemia
- Severe ventricular dysfunction
- Peripheral vascular disease
- Concomitant use of:
- Beta-blockers (bradycardia)
- Tricyclic antidepressants (counteract effect)
- Digoxin (bradycardia)
- Haloperidol (prolongation of QT interval)
- Sudden withdrawal should be avoided due to the risk of rebound hypertension
- IV Injection:
- May be given undiluted or diluted to aid slow administration
- IV infusion:
- Suggested standard infusion in critical care
- Dilute to 15mcg/ml or 30mcg/ml
- Sodium chloride 0.9% or glucose 5% can be used
- IV Injection:
- May be given undiluted or diluted to aid slow administration
- IV infusion:
- Suggested standard infusion in critical care
- Dilute to 15mcg/ml or 30mcg/ml
- Sodium chloride 0.9% or glucose 5% can be used
Physico-Chemical Properties
Molecular Structure
- Imidazoline derivative
- Chemical name is 2-((2,6-dichlorophenyl) amino)-2-imidazoline hydrochloride
- Chemical formula is C9H9Cl2N3
Chemical Properties
- Basic molecule with pKa 8.06
- Highly lipophilic due to dichlorophenyl ring
Pharmacokinetics
- IV: 5-7 minutes
- PO: 1-2 hours
- IV: 3-7 hours
- PO: Up to 8 hours
- Absorption is rapid, with peak plasma levels within 1-2 hours
- Readily crosses the blood-brain and placenta barriers
- Around 40% metabolised in the liver
- Remaining is excreted unchanged by the kidneys
- Produces inactive metabolites
- Excreted renally (95%) and faecally (4%)
Significantly increased in renal failure (up to 23 hours)
Pharmacodynamics
- Selective agonist at presynaptic alpha-2 adrenoceptors:
- Less selective than dexmedetomidine with ratio of alpha-1:alpha-2 1:200
- Acts particularly on the locus coeruleus in the floor of the fourth ventricle, producing depression of thalamic transmission to the cerebral cortex
- Primarily responsible for sedation, anxiolysis and analgesia
- Reduce sympathetic outflow resulting in hypotension and bradycardia
- Some activity at alpha-1 receptors:
- Produces vasoconstriction at higher doses
- Produces centrally mediated hypotension
- Selective agonist at presynaptic alpha-2 adrenoceptors:
- Less selective than dexmedetomidine with ratio of alpha-1:alpha-2 1:200
- Acts particularly on the locus coeruleus in the floor of the fourth ventricle, producing depression of thalamic transmission to the cerebral cortex
- Primarily responsible for sedation, anxiolysis and analgesia
- Reduce sympathetic outflow resulting in hypotension and bradycardia
- Some activity at alpha-1 receptors:
- Produces vasoconstriction at higher doses
- Produces centrally mediated hypotension
- Sedation and anxiolysis:
- Effects comparable to normal sleep
- May be more co-operative and communicative than patients sedated with other drugs
- Decreases cerebral blood flow, but does not lower intracranial pressure
- Decreases intraocular pressure
- Decreases gastric and small bowel motility
- Acts as an antisialogogue
- Very minimal respiratory depression
- At therapeutic doses no change in respiratory rate or PaCO2
- Usually exerts biphasic effect on blood pressure:
- Causes hypotension at lower doses due to predominate effects on imidazoline and alpha-2 receptors
- Higher doses stimulate peripheral alpha-1 receptors, thereby causing vasoconstriction, which may increase blood pressure
- May cause a decrease in heart rate (average response 20% decrease)
- No effect on cardiac contractility, and the cardiac output is well maintained
- Acts as a diuretic due to inhibition of ADH
- Excessive sedation, confusion, hallucinations
- Hypotension (initial transient hypertension on injection)
- Bradycardia, heart block
- Dry mouth
- Constipation
- Excessive sedation, confusion, hallucinations
- Hypotension (initial transient hypertension on injection)
- Bradycardia, heart block
- Dry mouth
- Constipation
Clinical Essentials
- Intravenous Alpha-2 agonist with sedative and analgesic effects
- Produces sedation without significant effect on respiratory drive
- Produces less hypotension and has a more predictable haemodynamic profile than clonidine
- Primarily used in intensive care and anaesthesia due to the requirement for administration as an intravenous infusion
- Intravenous Alpha-2 agonist with sedative and analgesic effects
- Produces sedation without significant effect on respiratory drive
- Produces less hypotension and has a more predictable haemodynamic profile than clonidine
- Primarily used in intensive care and anaesthesia due to the requirement for administration as an intravenous infusion
Sedation on critical care
- Sedation of intubated and mechanically ventilated patients as a sole agent or as an adjunct to others:
- May reduce days of ventilation
- May reduce rates of delirium
- Treatment of agitated and delirious patients
- Must be weaned gradually
IV Infusion: 0.2-0.7 mcg/kg/hr (can increase cautiously to 1.5 mcg/kg/hr)
Adjunct to anaesthesia
- Reduces MAC of volatile agents
- Has some analgesic properties (reduces opiate requirement)
- Reduces postoperative nausea
- Reduces emergence delirium
IV Infusion: 0.2-0.7 mcg/kg/hr (can increase cautiously to 1.5 mcg/kg/hr)
Procedural sedation
- Useful for awake intubation
Adjunct to regional anaesthesia
- Prolongs duration of effect
- Useful in peripheral nerve, epidural, caudal and spinal blocks
- No definitive contraindications
- Extreme caution should be exercised in patients with:
- Heart block
- Bradycardia
- Hypotension or hypovolaemia
- Severe ventricular dysfunction
- Peripheral vascular disease
- Concomitant use of:
- Beta-blockers (bradycardia)
- Tricyclic antidepressants (counteract effect)
- Digoxin (bradycardia)
- Haloperidol (prolongation of QT interval)
- Caution should be exercised when using as a sole sedative agent in patients <65 years of age (signal toward worse outcomes)
- Sudden withdrawal should be avoided due to the risk of rebound hypertension
- No definitive contraindications
- Extreme caution should be exercised in patients with:
- Heart block
- Bradycardia
- Hypotension or hypovolaemia
- Severe ventricular dysfunction
- Peripheral vascular disease
- Concomitant use of:
- Beta-blockers (bradycardia)
- Tricyclic antidepressants (counteract effect)
- Digoxin (bradycardia)
- Haloperidol (prolongation of QT interval)
- Caution should be exercised when using as a sole sedative agent in patients <65 years of age (signal toward worse outcomes)
- Sudden withdrawal should be avoided due to the risk of rebound hypertension
- Suggested standard infusion in critical care
- Dilute to 4mcg/ml or 8mcg/ml
- Sodium chloride 0.9% or glucose 5% can be used
- Suggested standard infusion in critical care
- Dilute to 4mcg/ml or 8mcg/ml
- Sodium chloride 0.9% or glucose 5% can be used
Physico-Chemical Properties
Molecular Structure
- Imidazoline derivative
- Dextroisomer of the veterinary sedative medetomidine
- Chemical name is (S)-4-[1-(2,3-Dimethylphenyl)ethyl]-3H-imidazole
- Chemical formula is C13H16N2
Chemical Properties
- Basic molecule with pKa 7.1
- Freely soluble in water, but also has excellent fat solubility
Pharmacokinetics
- <5 minutes following loading & infusion)
- Within 15 minutes following loading & infusion
- Given as infusion
- Favourably short, up to 4 hours after prolonged infusion
- Extensive first-pass metabolism
- Primarily limited to intravenous use but can be given intranasally
(albumin and α1-glycoprotein)
- Readily crosses the blood-brain and placenta barriers
- Primarily metabolised in the liver
- Metabolised via glucuronidation and cytochrome 450 hydroxylation
- Metabolised to inactive metabolites
- Excreted renally (95%) and faecally (4%)
(rapid distribution phase)
Pharmacodynamics
- Selective agonist at presynaptic alpha-2 adrenoceptors:
- More selective than clonidine with ratio of alpha-1:alpha-2 1:1,620
- More pronounced effect on central alpha-2 receptors
- Acts particularly on the locus coeruleus in the floor of the fourth ventricle, producing depression of thalamic transmission to the cerebral cortex
- Primarily responsible for sedation, with more potent sedative effect than clonidine
- Reduces sympathetic outflow resulting in hypotension and bradycardia
- Some limited activity at alpha-1 receptors
- Some limited activity at imidazole receptors (though less than clonidine)
- Selective agonist at presynaptic alpha-2 adrenoceptors:
- More selective than clonidine with ratio of alpha-1:alpha-2 1:1,620
- More pronounced effect on central alpha-2 receptors
- Acts particularly on the locus coeruleus in the floor of the fourth ventricle, producing depression of thalamic transmission to the cerebral cortex
- Primarily responsible for sedation, with more potent sedative effect than clonidine
- Reduces sympathetic outflow resulting in hypotension and bradycardia
- Some limited activity at alpha-1 receptors
- Some limited activity at imidazole receptors (though less than clonidine)
- Sedation and anxiolysis:
- Effects comparable to normal sleep
- May be more co-operative and communicative than patients sedated with other drugs
- Decreases cerebral blood flow, but does not lower intracranial pressure
- Decreases intraocular pressure
- Decreases gastric and small bowel motility
- Acts as an antisialogogue
- Very minimal respiratory depression
- At therapeutic doses no change in respiratory rate or PaCO2
- May cause vasoconstriction, hypertension and reflex bradycardia if given as a bolus (boluses not recommended)
- At therapeutic doses central effect on sympathetic outflow causes:
- Bradycardia (average response 20% decrease)
- Vasodilation and hypotension (effects more predictable than clonidine)
- No effect on cardiac contractility, and the cardiac output is well maintained
- Acts as a diuretic due to inhibition of ADH
- Excessive sedation, confusion, hallucinations
- Hypotension (initial transient hypertension on injection)
- Bradycardia, heart block
- Dry mouth
- Constipation
- Excessive sedation, confusion, hallucinations
- Hypotension (initial transient hypertension on injection)
- Bradycardia, heart block
- Dry mouth
- Constipation

