RESOURCES
Review Articles
- Tameem et al, BJA Ed (2013); Cerebral Physiology
- Das et al, Anaes Int Care (2019); Applied cerebral physiology
- Sakka et al, Eur Ann Otorhinolaryngology (2011); Anatomy and physiology of cerebrospinal fluid
- Shatzmiller et al, J Neur Dis & Stroke (2016); Blood-Brain Barrier Crossing for Therapeutic and Diagnostic Agents
OBJECTIVES & QUESTIONS
Fundamentals
What is cerebrospinal fluid (CSF)?
- Specialized transcellular fluid that surrounds the brain and spinal cord
- Circulates within the cerebral ventricular system and the subarachnoid space
What are the functions of cerebrospinal fluid (CSF)?
Mechanical Protection
- Provides buoyancy and cushioning
- Reduces the effective weight of the brain
- Protects against deformation caused by acceleration and deceleration
Maintenance of Constant Environment
- Maintains a constant ionic and osmotic environment for neuronal cells
- Essential for the functioning of normal neuronal activity
Regulation of ICP
- Displacement of CSF into spinal canal provides important, though limited, compensation for increases in ICP ('Spatial compensation')
Control of Respiration
- Central chemoreceptors detect changes in CSF pH caused by variations in CO2 levels resulting in the respiratory centre adjusting respiratory rate and tidal volumes
- CO2 freely dissolves in CSF from blood given its lipid solubility and low molecular weight
- Comparatively low protein levels in CSF reduce buffering capacity making CSF pH very sensitive to changes in blood pCO2
Clearance of Waste Products
- The brain lacks a lymphatic system to cleat waste products (extracellular proteins excess fluid and metabolic waste)
- A specialised 'glymphatic system' circulates CSF in paravascular channels where waste products are removed
What is the normal volume of cerebrospinal fluid (CSF)?
- Overall volume is between 100-150ml
- 2⁄3 within the ventricles
- 1⁄3 within the subarachnoid space around the spinal cord (35ml)
- Equates to ~10% of intracranial volume
What is the pressure of cerebrospinal fluid (CSF)?
- CSF pressure is gravitational and varies with position
- In the lateral position normal pressure is 5-20 cm of H2O
- In the sitting position:
- Pressure in the lumbar region rises to 20-50 cmH20
- Pressure in the cervical region may be sub-atmospheric
Production & Reabsorption
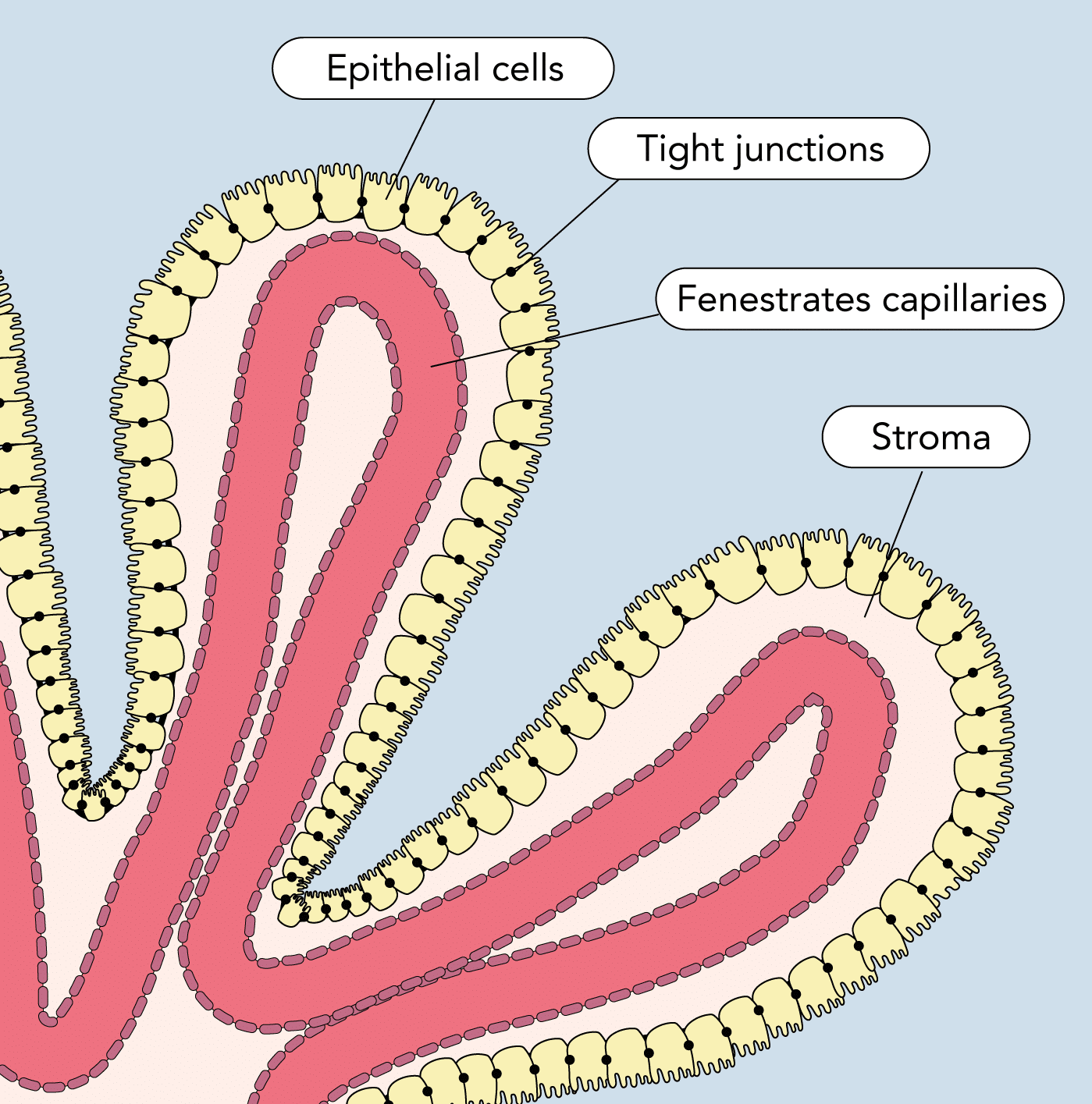
Where is CSF produced and through which processes?
- Produced by the four choroid plexuses:
- Located in the two lateral, third, and fourth ventricles
- Highly vascular invaginations of pia mater
- Covered by specialised ciliated ependymal cells
- Produced by a combination of:
- Filtration of plasma through the fenestrated capillaries
- Active transport of solutes
- Control of substances entering is regulated by the blood-CSF barrier (distinct from the BBB)
How much CSF is normally produced?
- Normal rate of production is 0.3-0.4ml/min or 20ml/hour or 500ml/day
- Results in effective replacement of CSF volume 3x daily
- Production is largely independent of ICP:
- Raised ICP is compensated by increased absorption of CSF reducing total volume
- Decreased when CPP <70 mmHg due to reduction in choroid plexus blood flow
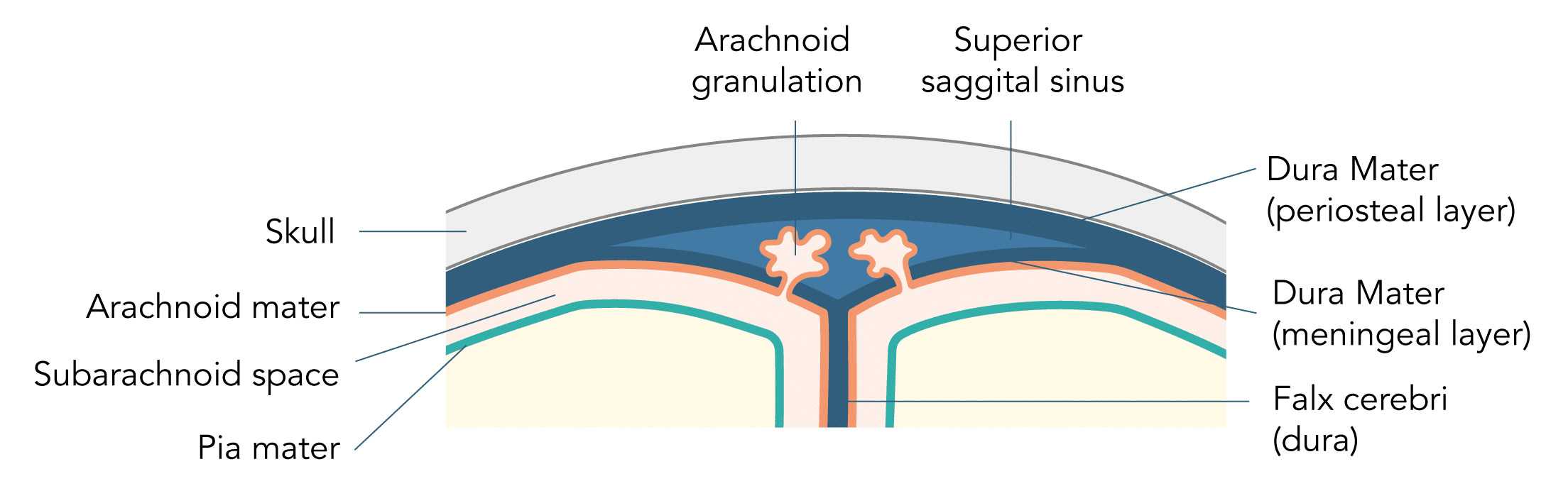
How and where is CSF reabsorbed?
- Reabsorbed by the arachnoid granulations:
- Villi arising from the arachnoid mater
- Project into venous sinuses and veins
- Reabsorption occurs throughout the brain and spine
- 90% by villi of the sagittal and sigmoid Dural sinuses
- 10% by spinal villi
- Reabsorption due to differences in pressure between CSF and veins
- Pressure of CSF typically 15 cm H2O and venous blood typical 8cm H2O
- Removal of CSF increases with rising intracranial pressure.
Composition
How does the makeup of CSF compare with plasma?
- Despite their common origin, CSF and plasma have a number of important differences:
- Na+, Cl– and Mg2+concentrations are higher
- K+ and Ca2+ concentrations are lower than plasma
- Protein is <1% of plasma resulting in reduced buffering capability and a lower pH
CSF
Plasma
Sodium
(mmol/L)
(mmol/L)
140
140
Calcium
(mmol/L)
(mmol/L)
1.2
(∼50% that of plasma)
(∼50% that of plasma)
2.2-2.6
Potassium
(mmol/L)
(mmol/L)
3.0
4.0-5.0
Chloride
(mmol/L)
(mmol/L)
120
96-106
Bicarbonate
(mmol/L)
(mmol/L)
24
Equal
Equal
24
Glucose
(mmol/L)
(mmol/L)
4
(∼60% that of plasma)
(∼60% that of plasma)
6
pCO2 (kPa)
6.6
5.2
pH
7.32
(0.08 lower than plasm)
(0.08 lower than plasm)
7.40
Protein
(g/L)
(g/L)
0.2-0.4
(<1% that of plasma)
(<1% that of plasma)
70
Specific Gravity
1.004-1.007
1.010
WCC
(per mm3)
(per mm3)
0-5
(usually lymphocytes and monocytes)
(usually lymphocytes and monocytes)
4,000-11,000
Ventricular System & CSF Flow
What is the structure of the ventricular system?
How does CSF flow through the ventricular system?
- Cerebrospinal fluid (CSF) is produced by the choroid plexuses of the lateral, third and fourth ventricles
- Passes from the lateral ventricles to the third ventricle through the two interventricular foramina (foramen of Monro)
- passes from the third ventricle to the fourth ventricle via the Sylvian aqueduct
- Escapes into the cerebellar subarachnoid space through the:
- Foramen of Magendie (Medial)
- Foramen of Lushka (Lateral)
- CSF then flows around the cerebral hemispheres and spinal cord
- Flow is aided by the ciliary movement of ependymal cells
- Reabsorbed primarily by the arachnoid villi of the dural venous sinuses
Structure
What is the blood brain barrier?
The unique anatomical and physiological properties of the central nervous system microvasculature that allows it to tightly regulate the movement of molecules, ions, and cells between the blood and the CNS
Which structures make up the blood-brain barrier?
- Comprises of 3 cellular layers and a basement membrane
- Together these form a barrier virtually impenetrable barrier to lipophobic molecules
Capillary Endothelium
- Interconnected by tight junctions (50-100x 'tighter' than peripheral capillaries) restricting the passage of substances from the capillaries to the brain ECF
- Differ from extracerebral capillaries in having a high density of mitochondria
- Have a relative paucity of pinocytic vesicles for vesicular transport
Basement Memebrane
- Surrounds the endothelium
- 40-50nm thick
- Rich in proteoglycans, heparin sulphate, collagen type IV and laminin
Pericytes
- Reside next to capillaries
- Possesses smooth muscle like action
Astrocytes
- A type of supportive glial cell
- Projections called foot processes ensheath >95% of vessel surface
- Secrete chemicals that reduce the permeability of the capillary endothelial cells
How does the endothelium of the blood brain barrier compare other with that at other sites?
Continuous Non-Fenestrated (General)
Continuous Non-Fenestrated (Blood-Brain Barrier)
Continuous Fenestrated
Non-continuous (Sinusoidal)
Muscle, thymus, bone, lung
Brain
Kidney
Liver
- Continuous endothelial cytoplasm without fenestrae and continuous basement membrane which restricts passage of substances across the endothelium
- Tight junctions between cells limiting paracellular movement of, ions, solutes, and water - regulation of transport varies across endothelium and influenced by both physiological and pathophysiological stimuli
- Vesicles transport substances through cytoplasm in a bidirectional pathway (transcytosis)
- Similar baseline characteristics to general non-fenestrated endothelium
- Possess very 'restrictive' tight junctions between cells to prevent paracellular transport
- Close contact with pericytes and astroctyes which aid barrier function
- Circular pores of fenestrae that penetrate the endothelium
- Thick continuous basement membrane
- Allows the passage of small macromolecules through the endothelium
- Does not form a continuous lining between the lumen and surrounding tissues
- Gaps between adjacent cells and absent basement membrane
- Poses no barrier to blood and constituents
Which structure in the brain lie outside the blood-brain barrier?
- Certain areas of the brain have a reduced blood-brain barrier and retain a direct connection with the systemic circulation in order to
- Detect alterations in composition of the blood
- Allow secretion of hormones
- Areas that are outside the BBB are known as ‘circumventricular organs’:
Hypothalamus
- Hypothalamic osmoreceptors monitor the osmolarity of systemic blood
Area postrema
- Contains a chemoreceptor trigger zone
- In the presence of noxious substances, sends afferent signals to the vomiting centre triggering vomiting
Anterior & posterior pituitary gland
- Secretes eight pituitary hormones directly into the systemic circulation
Choroid plexus
- Uses plasma from systemic blood to produce CSF
Pineal gland
- Secretes melatonin directly into the systemic circulation.
Subfornical organ
- Contains a chemoreceptor area
- Monitors blood angiotension II leveI as part of the regulation of body fluids
Function
What are the functions of the blood-brain barrier?
Barrier Functions
- Protects against potentially harmful molecules from entering the brain
- Provided through 4 main mechanisms:
- Paracellular barrier: endothelial tight junction restrict free movement of water
- Transcellular barrier: Low level of inherent endocytosis and transcytosis prevents transport of substances to the cytoplasm
- Enzymatic barrier: Complex set of enzymes capable of metabolising compounds before crossing the BBB
- Efflux barrier: Large number of efflux transporters present which can remove molecules from cells of the BBB
Carrier Functions
- Transports nutrients, metabolites and essential ions to ensure the maintenance of a constant environment for the functioning of neurons
- Provided through a number of mechanisms:
- Passive and facilitated diffusion: Allows small lipid soluble molecules, water and gases to pass through the membrane
- Specific transport proteins: Provides a supply of essential nutrients such as glucose and amino acids
- Transcytosis: Ensures important metabolic molecules such as insulin can reach the brain
How do substances cross the blood-brain barrier and which substances pass by each route?
Route
Examples
Free Membrane Diffusion
Small Lipophilic molecules and gases:
- O2, CO2
- Anaesthetics
- Ethanol, nicotine
Membrane Channels
Small ions and water:
- H2O
- Na, K+, Cl-
Carrier-Mediated Transport
- Energy transport systems:
- Glucose (GLUT-1)
- Lactate, pyruvate (MCT1)
- Creatine (CrT)
- Amino acid transport systems
- Large neural amino acids (LAT1)
- Neurotransmitter precursors
Receptor-Mediated Transport (via transcytosis)
- Insulin
- Leptin
- IgG
- TNFa
Adsorption mediated transport (via transcytosis)
- Histone
- Albumin
Which factors can increase the rate of transfer of substances across the blood brain barrier?
Factors that increase the rate of transfer across the blood–brain barrier include:
- High lipid solubility
- Low degree of ionisation
- Low protein binding
- Low molecular weight
- High plasma–brain concentration gradient
Which substances does the blood-brain barrier prevent from entering the brain?
Catecholamines
- A number of catecholamines (such as noradrenaline and dopamine) act as neurotransmitters in the central nervous system
- Unregulated entry across the blood brain barrier can result in permanent neuroexcitatory damage
Amino acids
- Similarly to catecholamines a number of amino-acids (such as glycine and glutamic acid) act as neurotransmitters in the central nervous system
- Unregulated entry across the blood brain barrier can result in permanent neuroexcitatory damage
Ammonia (NH3)
- Ammonia is potentially neurotoxic in significant concentrations
- It is a small lipophilic molecule which may be expected to cross the BBB
- It is rapidly metabolised by the enzymatic barrier to glutamine, preventing passage across the BBB in relevant quantities
Macromolecules
- Plasma proteins such as albumin and plasminogen are damaging to nervous tissue and can lead to apoptosis
- The BBB prevents passage of such molecules leading to low CSF levels
- Results in a lower ability to buffer changes in pH
Charged Ions
- The BBB is impermeable to H+ and HCO3- ions due to their charge
- However it is permeable to CO2 which can pass freely through into the CSF
- In this way CO2 from arterial blood can become converted in to H+ and HCO3- ions which become trapped lowering the pH of CSF
Which important drugs pass freely through the blood-brain barrier?
Opioid Analgesics
- Morphine
- Codeine
- Fentanyl
Anaesthetic Agents
- Propofol
- Fentanyl
- Ketamine
- Volatile anaesthetics
Anetiepileptics
- Benzoziazepines
- Barbiturates
- Phenytoin
Antidepressants
- Triciylic antidepressants
- SSRIs
- MOAs
CNS Stimulants
- Cocaine
- Amphetamines
- MDMA
Antibiotics
- Carbapenems
- 3rd & 4th generation cephalosporins
- Fluoroquinolones
- Aciclovir
How can the passage of drugs to the CNS across BBB be enhanced?
Route
Explanation
Example
Bypass the BBB
- Direct administration into the CSF bypasses the BBB to reach structures within the CNS
- Intrathecal antibiotics to treat meningitis or ventriculitis
- Intrathecal chemotherapy agents to treat CNS malignancy
Increase the lipophilicity of drug
- Increased lipophilicity of aids passive diffusion across lipid membranes of the BBB
- Heroin has to acetyl groups added to morphine molecule making it 100x more lipid soluble - produces more rapid onset of action
- Once within the brain metabolised to morphine, which only slowly leaves the brain
Increase permeability of BBB
- Increased permeability my be due to disease or induced by vasoactive compounds (such as bradykinin and histamine) to enhance drug delivery
- Delivery of chemotherapeutic agents into the brain
- Delivery of certain antibiotics enhanced by inflammation in meningitis
'Prodrug' to Utilise BBB Transport Mechanisms
- Prodrugs which cross the BBB may be used which are subsequently metabolised in the brain to active compounds
- The neurotransmitter dopamine cannot cross the BBB
- The precursor L-DOPA is transported across the BBB by facilitated diffusion where it is subsequently converted to dopamine
- It is used in Patients with Parkinson’s disease, in which there is a dopamine deficiency of the substantia nigra
'Trojan Horse' Delivery to Utilise BBB Transport Mechanisms
- A monoclonal Ab (Mab) acts as a molecular Trojan horse to deliver drugs across the BBB
- A drug pharmaceutical is genetically fused to the MAb
- The MAb acts against receptors on cells of the BB such as the insulin receptor leading to transport across the cell via transcytosis
- Early clinical trials for specialist treatments