Time: 0 second
Question No. 2
Q: What are the functions of the pancreas?
Answer No. 2
Exocrine Functions
- Alkaline secretion to buffer gastric pH:
- Protects duodenal mucosa
- Produces optimal pH range for pancreatic enzymes
- Enzymatic digestion (Trypsin, Amylase, Elastase, Lipase)
Endocrine Functions
- Secretion of hormones to regulate blood sugar (Insulin, Glucagon, Somatostatin)
Question No. 3
Q: Which structures in the pancreas are dedicated to the endocrine and exocrine functions?
Answer No. 3
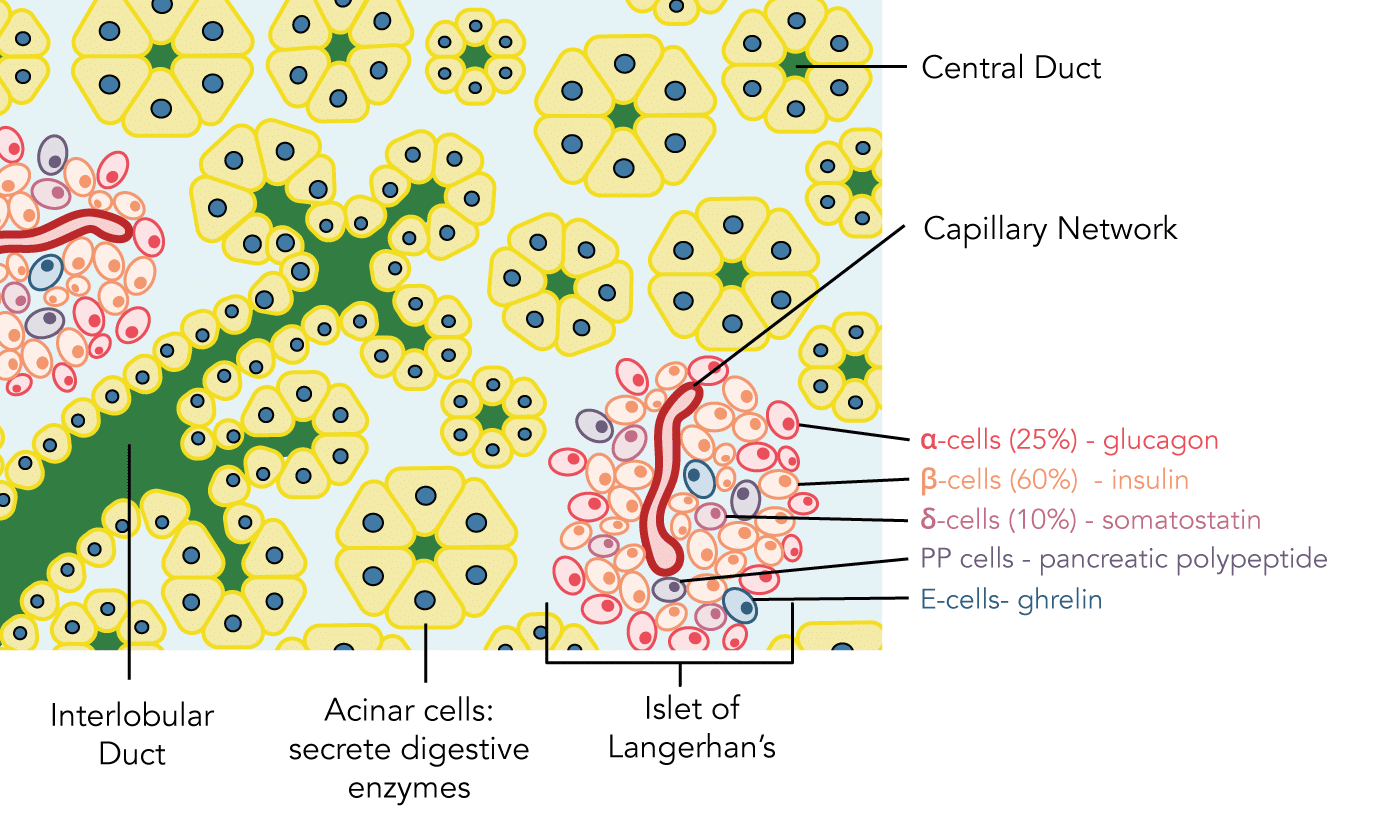
Microscopically divided in to exocrine and endocrine cells:
Exocrine Cells
- Vast majority of pancreatic tissue (99%)
- Acinar and ductal cells secrete alkaline digestive secretions containing enzymes
- Drain via pancreatic ductules and ducts which unite with the common bile duct opening in to the duodenum
Endocrine Cells
- Occupy on 1% of the pancreatic tissue
- Locates in collections called the "islets of Langerhans":
- Approximately 1 million scattered throughout acinar cells
- Possess different cell types which produce, store and secrete different hormones:
- α-cells (25%) - glucagon
- β-cells (60%) - insulin
- δ-cells (10%) - somatostatin
- PP cells - pancreatic polypeptide
- E-cells - ghrelin
Question No. 4
Q: Which digestive enzymes are produced by the pancreas and what are their functions?
Answer No. 4
Protein Breakdown
Protein Breakdown
- Trypsinogen
- Chymotrypsinogen
- Elastase
- Endopeptidases - cleave bonds between amino acids
- Split whole and partially digested proteins into peptides of various sizes but do not cause release of individual amino acids.
- Carboxypeptidase
- Aminopeptidase
- Exopeptidases - cleave bonds at the terminus of a peptide
- Splits peptides into individual amino acids, thus completing digestion of some proteins to amino acids.
Carbohydrate Breakdown
Carbohydrate Breakdown
- α-amylase
- Hydrolyses carbohydrates (starch and glycogen) to form mostly disaccharides and a few tri-saccharides.
- Has no activity against cellulose
Lipid Breakdown
Lipid Breakdown
- Pancreatic lipase
- Phospholipase
- Hydrolyses triglycerides and subsequently into monoglycerides and free fatty acids
Question No. 5
Q: What protects pancreatic tissue from digestive enzymes?
Answer No. 5
- Pancreatic enzymes are secreted in inactive form
- The suffix –ogen or prefix pro- indicates an inactive enzyme (e.g. trypsinogen, procarboxypeptidase
- They will be activated by:
- Enterokinase enzyme: secreted by the brush border of the duodenal wall when chyme comes into contact
- Autocleavage: by previously activated trypsin which can subsequently activate trypsinogen, chymotrypsinogen and procarboxypeptidase
- Acinar cells also secrete the enzyme trypsin inhibitor:
- Prevents activation of trypsin inside acini and ducts
- Protective ability can become overwhelmed if duct becomes blocked leading to autodigestion and acute pancreatitis
Question No. 6
Q: How are pancreatic secretions controlled?
Answer No. 6
- Minimal secretion between meals
- Entry of food stimulates secretions via neural and humoral mechanisms:
Neural
- Pancreas is innervated by the vagus nerve which releases acetyl choline
- When activated during the cephalic phase of digestion in anticipation of a meal, there is an increase in pancreatic acinar cell activity
Humoral (Hormonal)
Gastrin
- Secreted by the G cells of the stomach in response to gastric distension
- Functions include:
- Stimulation of pancreatic acinar cells to secrete digestive enzymes in preparation for the arrival of carbohydrates, proteins and fats
- Stimulation of gas gastric acid secretion by the parietal cells of the stomach
Cholecystokinin (CCK)
- Secreted by the duodenal mucosal cells in response to fat or protein rich chyme entering the duodenum
- Functions include:
- Increasing the production of bile in the liver
- Stimulation of gallbladder contraction
- Slowing gastric emptying
- Stimulation of the pancreatic acinar cells to secrete digestive enzymes
Secretin
- Secreted by the duodenal mucosa in response to the presence of acid-containing chyme in the duodenum
- Functions include:
- Slowing gastric emptying
- Stimulation of duct cells of the pancreas to secrete HCO ̅ to neutralise chyme
Question No. 7
Q: What are the phases of pancreatic secretion?
Answer No. 7
1. Cephalic Phase
- Describes the activity that occurs in anticipation of a meal
- Signals are transmitted from the brain via the vagus nerve causing release of acetylcholine in nerve endings in the pancreas
- Causes moderate amounts of enzymes to be secreted into the pancreatic acini, accounting for about 20 percent of the total secretion after a meal
- Only small amounts of water is secreted which limits flow of enzymes through ducts at this stage
2. Gastric Phase
- Continues neural stimulation of enzyme secretion continues, accounting for another 5 to 10 percent of pancreatic enzymes secreted after a meal
- Fluid secretion again remains small, limiting amount that reaches the duodenum
3. Intestinal Phase
- As chyme enters the small intestines the pancreatic secretions become copious
- Mainly in response to the hormone secretin
Question No. 8
Q: Which hormones are secreted by the endocrine pancreas and what are the functions?
Answer No. 8
Hormone
Production
Function
Insulin
Beta (ß) cells
- Acts to decrease plasma glucose levels (hypoglycaemic hormone)
- Promotes uptake especially into liver, muscles, and adipose tissue.
Glucagon
Alpha (α) cells
- Acts to increase plasma glucose levels (hyperglycaemic hormone)
- Promote hepatic glycogenolysis and gluconeogenesis
Somatostatin
Delta (δ) cells
- Inhibits the secretion of multiple hormones
- These include: growth hormone, insulin, glucagon, gastrin, vasoactive intestinal peptide (VIP), and thyroid-stimulating hormone
Ghrelin
Epsilon (E) cells
- Suppresses insulin via paracrine interaction with beta cells
- Stimulates appetite
- Stimulates growth hormone secretion
Amylin
Beta (ß) cells - co-secreted with insulin
- Suppresses glucagon via paracrine interaction with alpha cells
- Slows gastric emptying which delays absorption of glucose from the small intestine into the circulation
- Stimulates the satiety centre of the brain
Pancreatic Polypeptide
PP cells -previously upsilon (F) cells
- Function unknown
- Primarily used as marker for other pancreatic endocrine tumours
Question No. 9
Q: Describe the structure and synthesis of insulin?
Answer No. 9
Insulin
Structure, Sythesis & Transport
- A peptide hormone made of 51 amino acids
- Formed of 2 chains (α and β) connected by disulphide bridges
- Synthesised as proinsulin with chains joined by C-peptide
- C-peptide excised by endopeptidases in the endoplasmic reticulum of β cells prior to release
- C-peptide is 31 amino acid sequence has no known biological function
- Can be used as marker of endogenous insulin secretion
- Stored in secretory granules and is secreted by the cells via exocytosis
- It enters the portal system with half cleared by first pass through the liver
- Circulates entirely in an unbound form
Question No. 10
Q: What is the function of insulin and how does it exert it’s actions?
Answer No. 10
Function
- Key to glucose homeostasis - 'hypoglycaemic anabolic hormone':
- Liver:
- Promotes glycolysis and storage of glucose as glycogen (glycogenesis)
- Promotes conversion of glucose to triglycerides
- Muscle
- Promotes the uptake of glucose and its storage as glycogen
- Adipose tissue:
- Promotes uptake of glucose and its conversion to triglycerides for storage.
Mechanism of Action
- Binds to a specific receptor tyrosine kinase on the plasma membrane
- Increases its activity to of numerous numerous regulatory enzymes and promotes glucose transport in to cells by increasing membrane permeability
Question No. 11
Q: Describe the regulation of insulin secretion?
Answer No. 11
Regulation
Stimulated by:
- Raised plasma glucose
- Raised plasma fatty acid & ketone bodies
- Vagal nerve stimulation
- Amino acids
- Gut hormones (gastrin, secretin, CCK, and GIP)
Inhibited by:
- Sympathetic stimulation
- Somatostatin
