Time: 0 second
Question No. 2
Q: Which hormones are produced by the thyroid gland?
Answer No. 2
Hormone
Function
Thyroxine (T4) - carries 4 iodine atoms)
Regulation of metabolism and growth
Triiodothyronine (T3) - carries 3 iodine atoms)
Regulation of metabolism and growth
Reverse-triiodothyronine (r-T3) - formed by peripheral conversion of T3
Metabolically inactive
Calcitonin
Regulation of calcium and phosphate levels (lowers serum levels through deposition in bone and renal excretion)
Question No. 3
Q: How is thyroid hormone (T3 & T4) synthesised, stored and released?
Answer No. 3
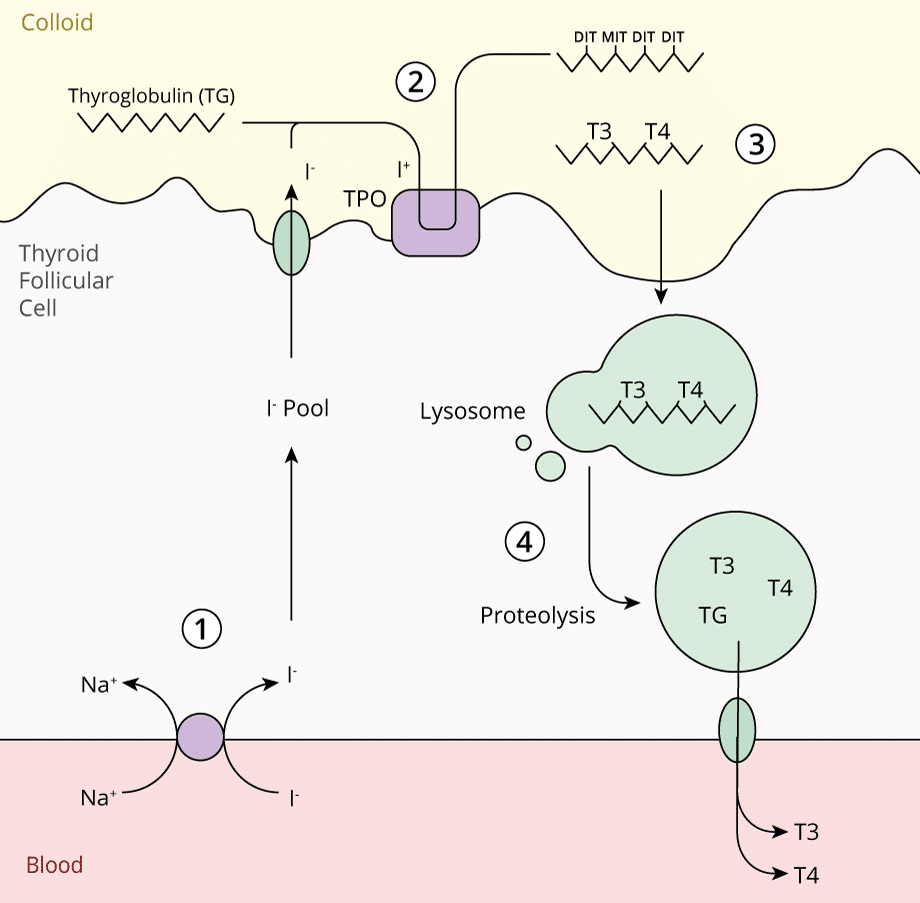
Can be considered in 4 steps:
1. Iodide Trapping
- Iodine obtained in diet from dairy, grains and meat (150mg/day required)
- Reduced to the inorganic form iodide (I-)
- Actively taken up by thyroid follicular cells, stimulated by TSH:
- Transported against a concentration gradient by Na+/I- Symporter (NIS)
2. Iodide Oxidation & Organification
- Moves apically in the cell where is oxidised to iodine (I+)
- Requires the membrane bound enzyme thyroperoxidase
- I+ covalently binds to tyrosine residues on thyroglobulin in the colloid
- May be iodinated at one or two positions forming:
- Monoiodotyrosine (MIT)
- Diiodotyrosine (DIT)
3. Storage in Colloid with Thyroglobulin
- Tyrosine residues couple to form precursors of thryroid hormones:
- MIT & DIT couple to form T3
- DIT & DIT couple to from T4
- T3 & T4 remain attached to the thyroglobulin molecule for storage in colloid
4. Secretion of Thyroid Hormones
- When stimulated by TSH, thyroglobulin is internalised into the thyrocyte membrane via endocytosis
- Lysosomal endopeptidase cleaves the thyroglobulin releasing T3 and T4
- Thyroid hormones are released into the cytoplasm and diffuse into the bloodstream through the basement membrane
Question No. 4
Q: What are the functions of thyroid hormone (T3 & T4)?
Answer No. 4
Effects on Metabolism
- Increase basal metabolic rate of most tissues (Long duration of action):
- Increased heat production
- Increases cardiac metabolic rate:
- Ionotropic / chronotropic effect
- Increased lipolysis & gluconeogenesis
Effect on Beta Receptors
- Increases number and sensitivity of B adrenoceptors
- Sensitises catecholamines
- Sensitises effects of insulin
- Increase in heart rate (HR) and myocardial contractility leading to an increase in cardiac output
Effect on Growth and Development
- Increases Growth hormone
- Vital in growth and development of nervous system:
- Neuronal myelination
- Nerve axon growth
Question No. 5
Q: Compare T3 and T4?
Answer No. 5
T3
- Active form of thyroid hormone - 3x more potent than T4
- 20% of T3 secreted directly from the thyroid
- 80% converted peripherally from T4
T4
- Often referred to as the prohormone due to low biological coactivity
- Approximately 90% is converted in peripheral tissues to more active T3 form - principally in the liver and kidneys
- Can also be converted to metabolically inactive reverse T3 (rT3)
- Fasting increases the ratio of rT3:T3.
Question No. 6
Q: What are the causes of hyperthyroidism?
Answer No. 6
Mechanism
Cause
Primary Hypothyroidism
Primary Hypothyroidism
Loss of functional thyroid tissue
- Autoimmune hypothyroidism:
- Hashimoto's
- Destructive thyroiditis
- Postpartum
- Subacute
- Iatrogenic - treatment for malignancy or hyperthyroidism
- Infiltrative disease (sarcoidosis)
Functional defects in thyroid hormone synthesis and release
- Iodine deficiency (Most common worldwide)
- Drugs (Amiodarone, lithium, interferon)
- Congenital syndromes
Secondary Hypothyroidism
Secondary Hypothyroidism
Loss of functional hypothalamic or pituitary tissue
- Hypopituitarism
- Congenital lesions
Functional defects in TSH synthesis and release
- Drugs (Dopamine, glucocorticoids)
- Congenital syndromes
Peripheral Hypothyroidism
Peripheral Hypothyroidism
Resistance to thyroid hormones
- Congenital syndromes
Question No. 7
Q: What are the clinical features of hyperthyroidism?
Answer No. 7
Hyperthyroidism is a multisystem disease:
General
- Tremor
- Weight loss
- Heat intolerance
- Diaphoresis
Cardiovascular
- Palpitations
- Tachycardia
- Atrial fibrillation
- High output cardiac failure (Dyspnoea, peripheral oedema)
Respiratory
- Tachypnoea
- Pulmonary hypertension
Neuromuscular
- Brisk reflexes
- Proximal muscle weakness
Neuropsychiatric
- Jitteriness
- Anxiety
- Insomnia
- Psychosis
Gastrointestinal
- Diarrhoea
Genitourinary
- Infertility
- Amenorrhoea
Cutaneous
- Onycholysis
- Hyperpigmentation
- Pretibial myxoedema*
- Thyroid acropachy*
Ophthalmic
- Exophthalmos*
- Periorbital oedema*
- Eyelid lag*
Other
- Goitre
* Pathognomonic of Grave's Disease
Question No. 8
Q: Which drugs have an anti-thyroid effect and what are their mechanisms?
Answer No. 8
Examples
Mechansims
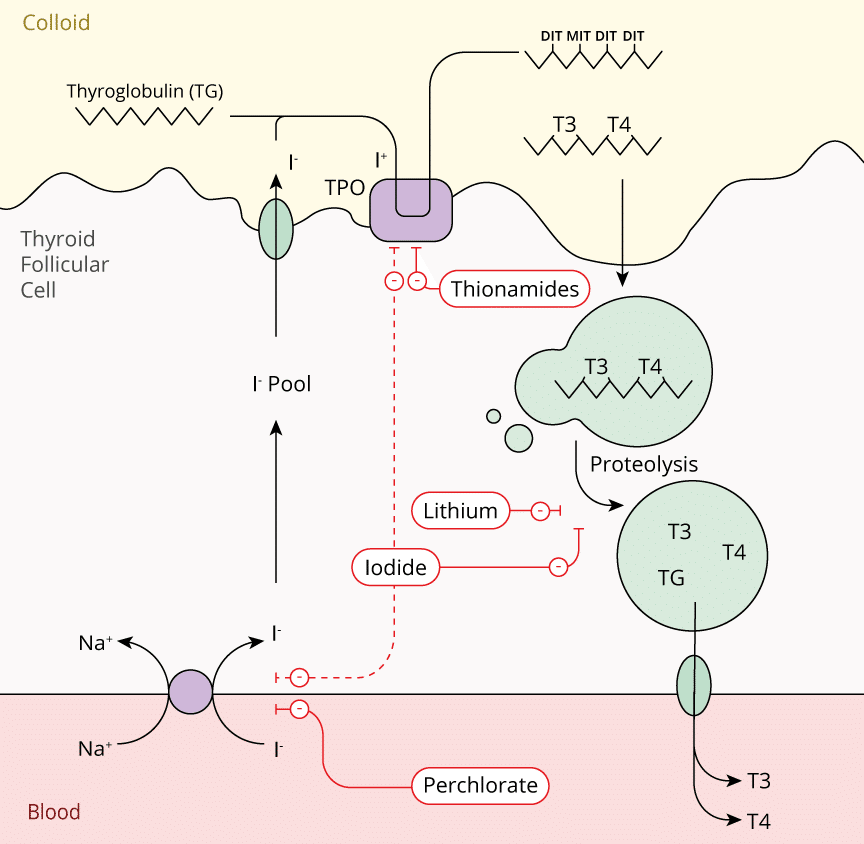
Inhibition of Ionic Trapping
- Thiocyanate
- Perchlorate
- Inhibition of the sodium-iodide symporter (NIS) on the thyroid follicular cell membrane.
Inhibition of Hormone Synthesis
- Thionamides:
- Propylthiouracil
- Carbimazole
- Methimazole
- Inhibition of thyroperixodase preventing organification or iodine
Inhibition of Hormone Release
- Iodides:
- Potassium Iodide (Lugol's Iodine)
- Sodium Iodide
- Increased resistance of thyroglobulin to proteolytic degradation
- (Iodides also prevent ionic trapping and hormone synthesis)
Prevention of Peripheral Conversion to Thyroid Hormone
- Corticosteroids
- Propranolol
- Propylthiouracil
- Amiodarone
- Radiocontrast media
- Increased type 3 deiodinase activity
Destruction of Thyroid Tissue
- Radioactive iodine (131,125,123)
Question No. 9
Q: Which drugs can be used to counteract the peripheral effects of thyroid hormones?
Answer No. 9
β-blockers (Propranolol, Esmolol)
- Standard of acute care - most of the immediately life-threatening consequences of thyroid storm are cardiovascular
- Effective in controlling heart rate; with a slower rate the cardiac failure may actually improve and the blood pressure may paradoxically increase
Diltiazem
- Effective at controlling heart rate in patients in which β-blockade is contraindicated such as asthma
Corticosteroids
- Thyroid disease (particularly long-standing hyperthyroidism) is associated with a diminished adrenal reserve
- Routinely used in thyroid storm to address the coexisting hypoadrenal state
Question No. 10
Q: Give some examples of thionamide drugs?
Answer No. 10
- Thiouracils:
- Propylthiouracil
- Imidazoles:
- Methimazole
- Carbimazole
Question No. 11
Q: What are the side effects of thionamide drugs?
Answer No. 11
Significant clinical side effects include:
- Agranulocytosis (<0.5%)
- Transient leucopaenia (10%)
- Mucocutaneous rash
- Hepatotoxicity
- Vasculitis