Time: 0 second
Question No. 2
Q: Describe the microscopic structure of the thyroid gland?
Answer No. 2
- Functional unit of the thyroid is the follicle:
- Outer sphere of cuboidal epithelial cells (thyrocytes) and thin basement membrane:
- Site of thyroglobulin production
- Filled with a protein rich core called colloid:
- Made up of thyroglobulin a large glycoprotein
- Serves as the main storage of thyroid hormones
- Outer sphere of cuboidal epithelial cells (thyrocytes) and thin basement membrane:
- C-cells are dispersed between follicles to produce calcitonin
Question No. 3
Q: Which hormones are produced by the thyroid gland?
Answer No. 3
Hormone
Function
Thyroxine (T4) - carries 4 iodine atoms)
Regulation of metabolism and growth
Triiodothyronine (T3) - carries 3 iodine atoms)
Regulation of metabolism and growth
Reverse-triiodothyronine (r-T3) - formed by peripheral conversion of T3
Metabolically inactive
Calcitonin
Regulation of calcium and phosphate levels (lowers serum levels through deposition in bone and renal excretion)
Question No. 4
Q: What are the functions of thyroid hormone (T3 & T4)?
Answer No. 4
Effects on Metabolism
- Increase basal metabolic rate of most tissues (Long duration of action):
- Increased heat production
- Increases cardiac metabolic rate:
- Ionotropic / chronotropic effect
- Increased lipolysis & gluconeogenesis
Effect on Beta Receptors
- Increases number and sensitivity of B adrenoceptors
- Sensitises catecholamines
- Sensitises effects of insulin
- Increase in heart rate (HR) and myocardial contractility leading to an increase in cardiac output
Effect on Growth and Development
- Increases Growth hormone
- Vital in growth and development of nervous system:
- Neuronal myelination
- Nerve axon growth
Question No. 5
Q: Compare T3 and T4?
Answer No. 5
T3
- Active form of thyroid hormone - 3x more potent than T4
- 20% of T3 secreted directly from the thyroid
- 80% converted peripherally from T4
T4
- Often referred to as the prohormone due to low biological coactivity
- Approximately 90% is converted in peripheral tissues to more active T3 form - principally in the liver and kidneys
- Can also be converted to metabolically inactive reverse T3 (rT3)
- Fasting increases the ratio of rT3:T3.
Question No. 6
Q: How is thyroid hormone (T3 & T4) synthesised, stored and released?
Answer No. 6
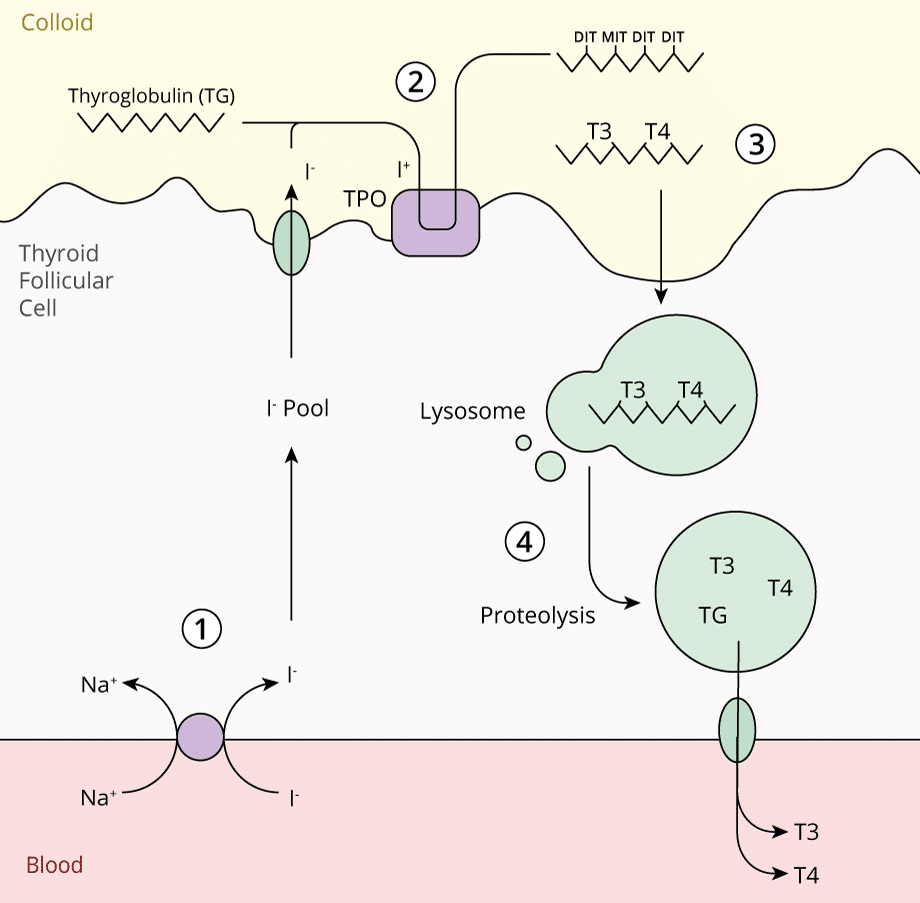
Can be considered in 4 steps:
1. Iodide Trapping
- Iodine obtained in diet from dairy, grains and meat (150mg/day required)
- Reduced to the inorganic form iodide (I-)
- Actively taken up by thyroid follicular cells, stimulated by TSH:
- Transported against a concentration gradient by Na+/I- Symporter (NIS)
2. Iodide Oxidation & Organification
- Moves apically in the cell where is oxidised to iodine (I+)
- Requires the membrane bound enzyme thyroperoxidase
- I+ covalently binds to tyrosine residues on thyroglobulin in the colloid
- May be iodinated at one or two positions forming:
- Monoiodotyrosine (MIT)
- Diiodotyrosine (DIT)
3. Storage in Colloid with Thyroglobulin
- Tyrosine residues couple to form precursors of thryroid hormones:
- MIT & DIT couple to form T3
- DIT & DIT couple to from T4
- T3 & T4 remain attached to the thyroglobulin molecule for storage in colloid
4. Secretion of Thyroid Hormones
- When stimulated by TSH, thyroglobulin is internalised into the thyrocyte membrane via endocytosis
- Lysosomal endopeptidase cleaves the thyroglobulin releasing T3 and T4
- Thyroid hormones are released into the cytoplasm and diffuse into the bloodstream through the basement membrane
Question No. 7
Q: How is thyroid hormone transported?
Answer No. 7
- <1% transported freely in plasma unbound to plasma proteins:
- Forms the active portion of the hormone
- Mostly transported by non-covalent binding to plasma proteins:
- Thyroid binding globulin (TBG) - predominant transport protein
- Transthyretin
- Albumin
- TBG has 10x the affinity for T4 than T3:
- Therefore T3 is more readily available and is removed from the circulation
Question No. 8
Q: What factors control the synthesis and secretion of thyroid hormone?
Answer No. 8
- Thyroid hormone production is regulated by a series of negative feedback loops
- Thyroid stimulating hormone (TSH) is an important regulator:
- Peptide hormone produced in the anterior pituitary gland
- Stimulates the production and release of thyroid hormones
- TSH production is stimulated by:
- TRH production
- Low serum levels of thyroid hormones
- TSH production is inhibited by:
- High serum levels of thyroid hormones (negative feedback loop)
- High serum levels of TSH (ultra-short negative feedback loop)
- Thyrotropin-releasing hormone (TRH) is another important regulator:
- Peptide hormone produce in the hypothalamus
- Stimulates the production and release of TSH
- TRH production is stimulated by:
- Low serum levels of thyroid hormones
- TRH production is inhibited by:
- High serum levels of thyroid hormones (negative feedback loop)
Question No. 10
Q: Where do portal circulations exist in the body?
Answer No. 10
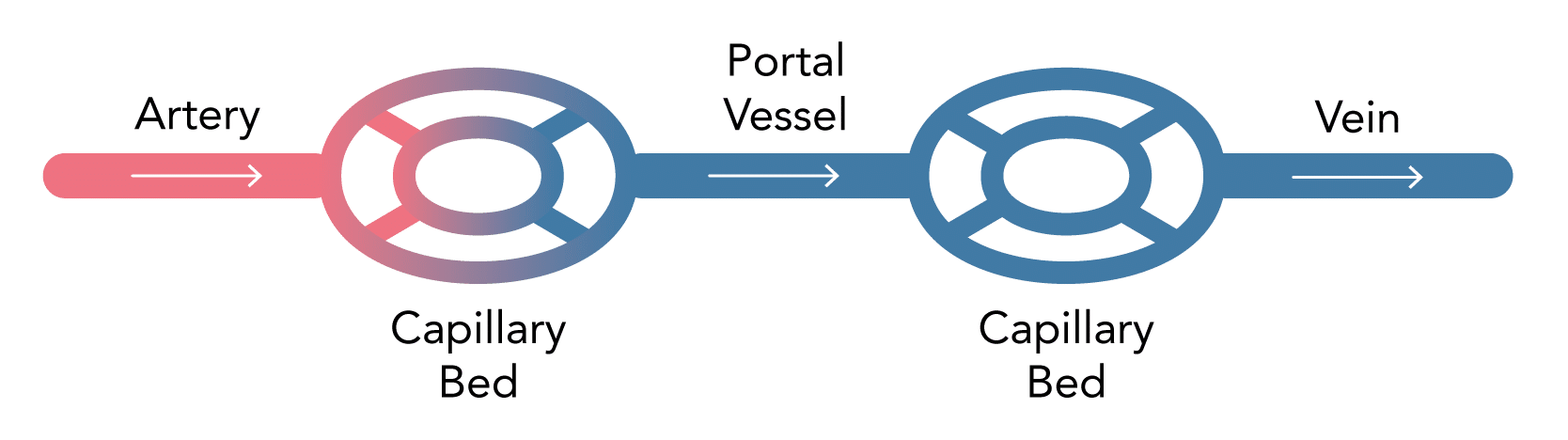
Three portal systems exist within the body:
- Hypothalamus & anterior pituitary gland
- Liver
- Kidneys (nephrons)
Question No. 11
Q: Why is the hypothalamic-pituitary axis a portal circulation?
Answer No. 11
Hypothalamus & Anterior Pituitary
- Blood vessels enter the hypothalamus and form a capillary network into which trophic releasing hormones are released
- Portal vessels communicate with the anterior pituitary gland providing a method of hormonal communication
- A second capillary network allows the action of trophic releasing hormones on pituitary cells and the subsequent release of organ specific hormones which are distributed around the body