Time: 0 second
SOE 069: Nausea & Vomiting
Introduction
You are assessing a 36-year-old lady preoperatively who is due to undergo a laparoscopic ovarian cystectomy. She has had one previous anaesthetic and developed vomiting postoperatively. You are asked to see her in the recovery room as she is having severe nausea and vomiting following her operation…
Question No. 2
Q: Can you define nausea, retching and vomiting?
Answer No. 2
Nausea: the sensation of the need to vomit
Vomiting: the involuntary, forceful expulsion of gastric contents via the mouth
Retching: the involuntary movements of vomiting without expulsion of vomitus
Question No. 5
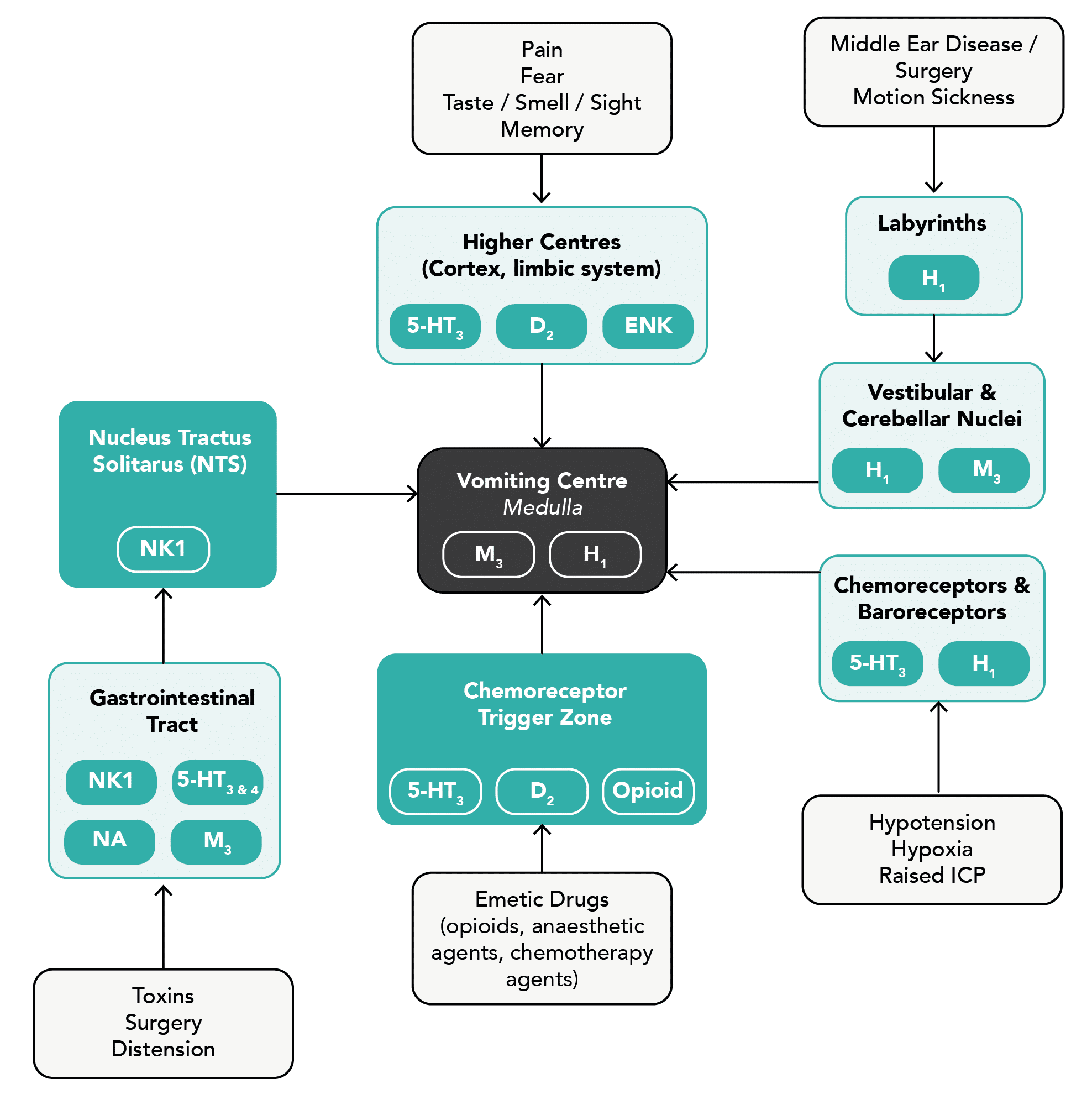
Q: Which receptors are involved in nausea and vomiting and which anti-emetic drugs act on them?
Answer No. 5
Receptor
Location
Drugs
Dopamine
(D2)
(D2)
- Chemoreceptor trigger zone
- Higher cortical centres
- Prochlorperazine
- Droperidol
- Haloperidol
- Metoclopramide
Serotonin
(5HT3 & 5HT4)
(5HT3 & 5HT4)
- Gastrointestinal tract
- Chemoreceptor trigger zone
- Higher cortical centres
- Ondansetron
- Granisetron
Histamine
(H1)
(H1)
- Vestibular apparatus
- Vomiting centre
- Cyclizine
- Promethazine
Neurokinin-1
(NK1)
(NK1)
- Gastrointestinal tract
- Nucleus tractus solitarus
- Vestibular apparatus
- Aprepitant
- Fosaprepitant
- Casopitant
Muscarinic Acetylcholine
(M3)
(M3)
- Gastrointestinal tract
- Vomiting centre
- Scopolamine (Hyoscine)
Noradrenaline
(NA)
(NA)
- Gastrointestinal tract
-
Opioid receptors
- Chemoreceptor trigger zones
-
Enkephalin
(ENK)
(ENK)
- Higher cortical centres
-
Question No. 6
Q: What is the chemoreceptor trigger zone (CTZ)?
Answer No. 6
- A group of cells close to the area postrema on the floor of the fourth ventricle
- Located outside the blood-brain barrier to detect toxins in the blood
- Extremely sensitive to emetic stimuli
- Dopamine and 5-HT receptors play an important role in the activity of the CTZ
Question No. 8
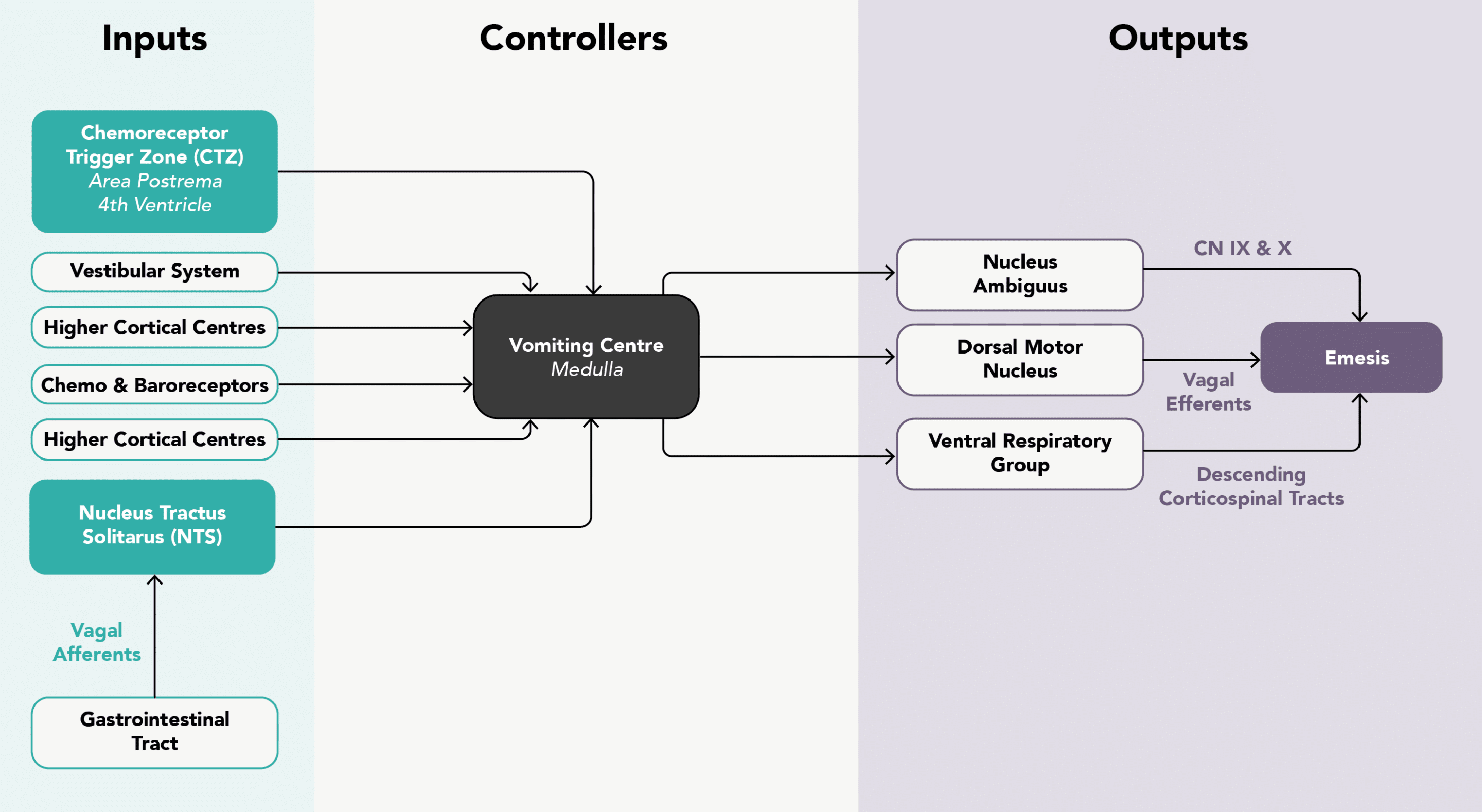
Q: How does the process of vomiting occur?
Answer No. 8
Can be considered as two separate stages:
Pre-Ejection Phase
- Symptoms of nausea occur
- Sympathetic stimulation:
- Tachycardia, tachypnoea, sweating
- Parasympathetic stimulation:
- Salivation
- Upper and lower oesophageal sphincters relax
- Retrograde peristalsis to the stomach
Ejection Phase
- Protection of the airway occurs:
- Respiration temporarily ceases mid-inspiration
- Hyoid and larynx rise to open crico-oesophageal sphincter
- Glottis closes and soft palate elevates to close posterior nasal space
- Soft palate elevates to close off the nasopharynx
- Ejection of gastric contents follows:
- Contraction of the abdominal muscles results in raised intra-abdominal pressure
- Gastro-oesophageal sphincter opens
Question No. 9
Q: What are the potential complications of vomiting?
Answer No. 9
- Simple vomiting rarely leads to medical complications
- Commonly leads to patient dissatisfaction following surgery
- However, severe cases can lead to:
- Increased length of hospital stay / delayed discharge
- Aspiration pneumonia
- Dehydration
- Metabolic alkalosis
- Electrolyte imbalance
- Increased bleeding
- Suture dehiscence
- Incisional hernias
- Oesophageal rupture
Question No. 10
Q: How is postoperative nausea & vomiting (PONV) defined?
Answer No. 10
Nausea, retching, or vomiting occurring in the recovery period or the immediate 24 hours postoperatively
Question No. 11
Q: What are the risk factors for developing PONV?
Answer No. 11
Patient Factors
- Female gender (x3 risk - biggest risk factor)
- Younger age
- Non-smoker
- History of PONV previously
- History of Motion sickness
- Preoperative anxiety
- Disease states:
- Uraemia
- Intestinal obstruction
- Hypoglycaemia
- Hypoxia
Anaesthetic Factors
- Use of specific drugs:
- Inhalational agents (2x risk, dose dependent)
- Nitrous oxide (1.4x risk, likely due to GIT / middle ear cavity distension)
- Opioids (note untreated pain is also emetogenic)
- Sympathomimetics
- Etomidate, ketamine, methohexitone (compared with propofol and thiopentone)
- Neostigmine (recent work suggests that this is not associated with PONV)
- Prolonged anaesthesia
- Spinal anaesthesia (blocks above T5)
- Intraoperative dehydration
- Inexperienced bag and mask ventilation (gastric dilatation)
Surgical Factors
- Specific surgery types:
- Abdominal surgery
- Laparoscopic surgery
- Intracranial surgery
- Middle ear surgery
- Squint surgery (highest incidence of PONV in children)
- Gynaecological
- Head and neck surgery - especially tonsillectomy and adenoidectomy
- Other surgical factors:
- Prolonged surgery
- Painful surgery