Question No. 2
Q: What is the surgical stress response?
Answer No. 2
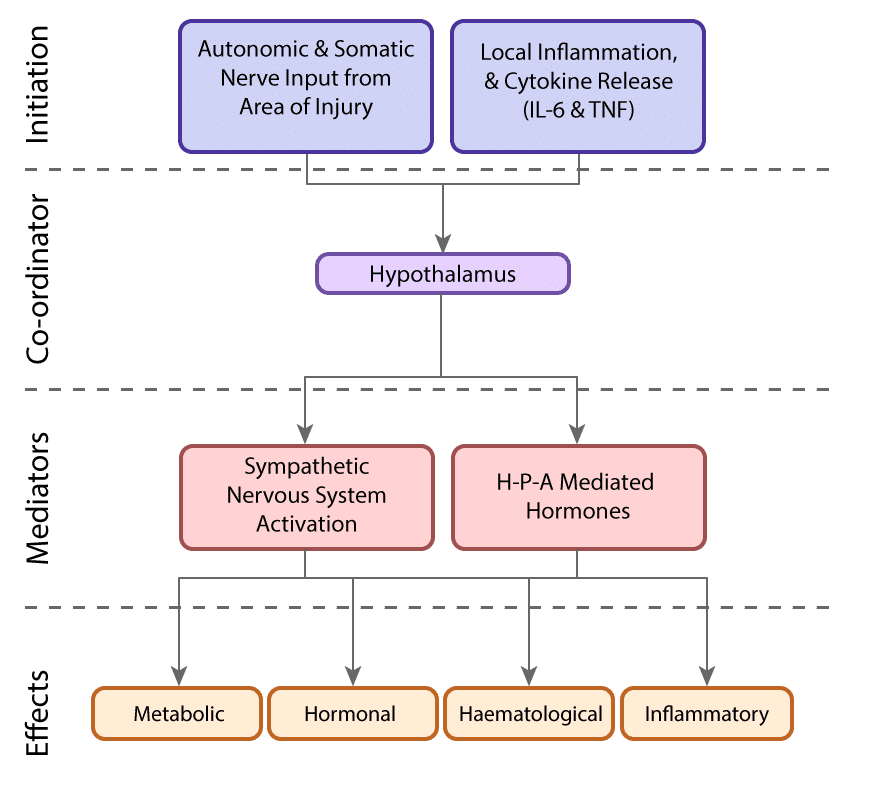
A group of complex neuroendocrine and metabolic changes that occur in response to trauma and surgery. The net effect is increased catabolism, substrate mobilisation and retention of salt and water
Question No. 4
Q: What are the hormonal sequelae of the stress response?
Answer No. 4
- Growth Hormone (GH)
- Adrenocorticotrophic Hormone (ACTH)
- β-Endorphin
- Prolactin
- Anti-diuretic hormone (ADH)
- Catecholamines
- Cortisol
- Aldosterone
- Glucagon
- Renin
- Thyroid-stimulating hormone (TSH)
- Luteinizing hormone (LH)
- Follicle-stimulating hormone (FH)
- Insulin
- Testosterone
- Oestrogen
- Tri-iodothyronine (T3)
Question No. 5
Q: What are the metabolic sequelae of the stress response?
Answer No. 5
- Blood glucose concentrations increase after trauma:
- Stimulated by cortisol and catecholamine
- Due to increased hepatic glycogenolysis and gluconeogenesis
- Peripheral glucose utilisation also decreases
- Increase in concentration proportional to the degree of injury
- Hyperglycaemia persists due during catabolic phase:
- Usual homeostatic mechanisms ineffective
- Hormones continue to promote glucose production
- Relative lack of insulin and peripheral insulin resistance observed
- Protein catabolism occurs to mobilise amino acids:
- Stimulated by cortisol
- Amino acids used for energy or converted to acute-phase proteins
- Predominantly skeletal muscle is broken down:
- Results in marked wasting and weight loss
- Visceral protein also catabolised:
- Can predispose to organ dysfunction
- Increased lipolysis mobilising triglycerides to glycerol and fatty acids
- Plasma levels may remain unchanged:
- Glycerol acts as substrate for gluconeogenesis in the liver
- Fatty acids re-esterized converted to ketone bodies
- Stimulated by cortisol, catecholamines and growth hormone
Question No. 6
Q: What are the phases of the stress response?
Answer No. 6
Classically described as three distinct phases:
Timing: < 24 hours
Characterized by reconstruction of the body’s normal tissue perfusion and efforts to protect homeostasis. In this phase, there is a decrease in total body energy and urinary nitrogen excretion.
- Initial period of shock:
- ↓ cardiac output
- Hypotension may occur
- Lactic acid accumulates
- Acute inflammatory response occurs at the site of injury:
- Release of cytokineso
- Systemic vasodilatation follows
- The body tries to preserve volume:
- Hypercoagulable state to reduce bleeding
- Activation of RAA system
- ↑ ADH secretion
- ↑ sodium retention and ↓ urine output
- Neuro-Endocrine changes:
- ↑ Activation of sympathetic nervous system
- ↑ catecholamines
- ↑ glucagon and ↓ insulin
- Mildly ↑ glucose
- Period of ↓ metabolism:
- ↓ BMR
- ↓ temperature
- Substrate is mobilised but not utilised
Timing: 2-8 days
Characterized by catabolism and volume replacement to provide a compensating response to the initial trauma. Response is directed to the supply of energy and protein substrates to repair damaged tissues and protect critical organ functions. While necessary for survival in the short term, it can become damaging for the body when the response is severe or long-lasting.- Period of hypermetabolism
- ↑ cardiac output
- ↑ O2 consumption
- Normal / high body temp
- Changes driven by:
- ↑ catecholamines
- ↑ Counterregulatory hormones
- ↑ cytokines
- Ongoing fluid & sodium retention to replenish volume:
- The third spacing of fluid occurs
- Widespread metabolic changes
- Carbohydrate metabolism
- ↑ Glycogenolysis
- ↑ Gluconeogenesis
- Insulin resistance of tissues•
- Hyperglycaemia
- Fat metabolism
- ↑ Lipolysis
- Free fatty acids used as energy substrate by tissues (except brain)
- Some conversion of free fatty acids to ketones in liver (used by brain)
- Glycerol converted to glucose in the liver
- Protein metabolism
- ↑ Skeletal muscle breakdown
- Amino acids converted to glucose in liver
- Shift toward production of acute-phase proteins
- Increased nitrogen excretion (negative nitrogen balance)
- Carbohydrate metabolism
Timing: 3-14 days
Characterized by the restoration of body weight, skeletal muscle mass and fat stores. Occurs following the period of catabolism, when the release of pro-inflammatory mediators has subsided, and is often associated with clinical improvement in patients such as increased appetite and mobility.
- Timing of transition depends on injury severity:
- 3–8 days after uncomplicated elective surgery
- Several weeks after severe trauma and sepsis
- Mediated by catabolic hormones:
- ↑ insulin
- ↑ growth hormone
- ↑ androgens
- Metabolic changes include:
- Gradual restoration of body protein and fat stores
- Transition to normal positive nitrogen balance
- Clinically coincides with
- ↑ diuresis
- ↑ appetite
- ↑ mobility
- Can last for several months after serious injury
Question No. 7
Q: What are the adverse consequences of the stress response?
Answer No. 7
- ↑ catecholamines and angiotensin II:
- Peripheral vasoconstriction, hypertension & tachycardiab>
- ↑ myocardial workb> with precipitation of myocardial ischaemia
- Increased myocardial oxygen demand, increasing risk of ischemia
- Splanchnic vasoconstrictionb> which may impact on healing of anastomoses
- ↓ cardiac muscle mass:
- Precipitation of arrhythmias
- Hyperglycaemiab>:
- Poor wound healing
- Wound infections
- Nosocomial infectionsb>
- ↑ mortality in critical illnessb>
- Risk of iatrogenic hypoglycaemia
- Protein catabolism
- ↓ skeletal muscle massb>:
- Immobility - thus increasing venous thromboembolism risk
- Precipitation of respiratory failure due to loss of respiratory muscle power
- Electrolyte disturbance - due to mineralocorticoid activity
- Hypokalaemia (common)
- Hypernatraemia
- Fluid overload:
- Precipitation of LV failure
- Wound breakdown
- Anastomotic leak
- ↑ risk of DVT & PE
- ↑ susceptibility to infections
Question No. 8
Q: How do the overall changes in the stress response compare with those seen in starvation?
Answer No. 8
A patient-centered, evidence-based, multidisciplinary team developed pathways for a surgical specialty and facility culture to reduce the patient’s surgical stress response, optimize their physiologic function, and facilitate recovery. These care pathways form an integrated continuum, as the patient moves from home, through the pre-hospital/preadmission, preoperative, intraoperative, and postoperative phases of surgery, and home again
Question No. 11
Q: When should an ERAS programme be used?
Answer No. 11
- NICE guidelines suggest that "an enhanced recovery programme be offered to people having elective major or complex surgery"
- The ERAS Society has published ERAS pathways for a wide range of surgical specialities including cardiac, thoracic, colorectal, breast, gynaecology, upper gastrointestinal and urology
Question No. 12
Q: What are the benefits of ERAS?
Answer No. 12
- Improved satisfaction
- Shorter hospital stay
- Faster recovery
- Faster return to work
- Fewer complications
- Reduced waiting times
- Reduced length of stay
- Reduced cost (cheaper)
- Quicker turnover - thus reduced waiting lists
- Improved relationship between primary care and hospital
- Better MDT dynamics