Time: 0 second
Question No. 3
Q: What is the most obvious abnormality on the chest x-ray?
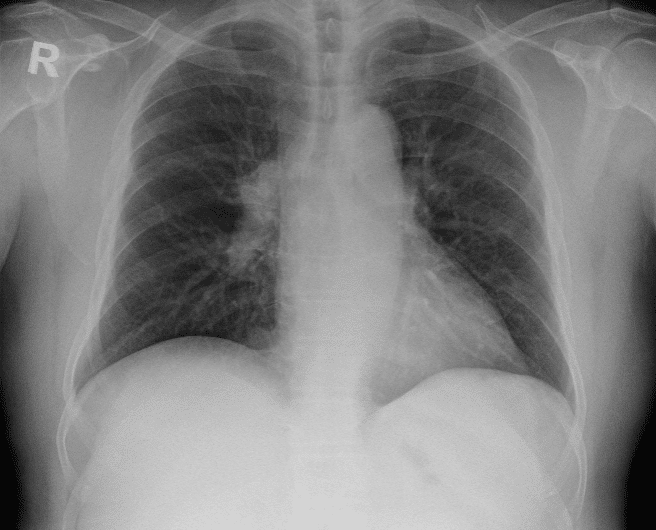
Answer No. 3
A right-sided hilar mass is present
Question No. 4
Q: What is the differential diagnosis for a unilateral hilar mass?
Answer No. 4
Infection
- Tuberculosis
- Lung Abscess
Inflammation
- Lymphadenopathy
Tumour
- Primary bronchogenic carcinoma
- Lymphoma
- Metastatic neoplasm
Vascular
- Pulmonary artery aneurysm / stenosis
Question No. 5
Q: How would you determine the diagnosis?
Answer No. 5
- Detailed clinical history & examination
- Full blood panel including infection and inflammation screen
- CT thorax (+/- PET scan)
- Bronchoscopy
- Biopsy (bronchoscopic or CT guided)
Question No. 7
Q: What approaches can be used for lung resection surgery be performed?
Answer No. 7
Approach
Description
UK Frequency
Open Thoracotomy
- Uses a large single incision (10-15cm) and rib spreading to gain entry to the chest
- Provides good vision and access to the lungs and mediastinum
- Forcible spreading of the ribs to permit the surgeons hands to enter results in great surgical access trauma and associated morbidity
- Significant risk of rib fractures and costovertebral joint damage
43.2%
Video-Assisted Minimal Approach (VATS)
- Uses a main incision (4-6cm), usually with multiple additional incisions, though single port entry is practiced
- Compared to open thoracotomy associated with significantly
- less postoperative pain, less intraoperative blood loss, shorter hospital stays and improved postoperative quality of life
- May offer more limited ability to perform extensive lymph node dissection though 5 years survival outcomes are non-inferior to open surgery
55.8
(10.6% conversion from open)
(10.6% conversion from open)
Robotic-Assisted Minimal Approach (RATS)
- Uses 3-4 small incisions to access the chest with robotic instruments
- Offers the theoretical advantage of 3-dimensional vision and instruments with 360-degree dexterity allowing increased ability to perform complicated proceduresAt present has comparable outcomes to VATS
55.8
(10.6% conversion from open)
(10.6% conversion from open)
Question No. 8
Q: How would you assess her fitness for lung resection?
Answer No. 8
- BTS recommends a tripartite risk assessment model when assessing fitness for lung resection surgery including:
- Risk of operative mortality
- Risk of perioperative myocardial events
- Risk of postoperative dyspnoea
- These can be used to discuss individual risks with the patient and MDT
Question No. 9
Q: What is the thoracascore?
Answer No. 9
- Thoracoscore is a global risk score used for estimating perioperative death in thoracic surgery
- Uses nine variables (age, sex, ASA score, performance status, dyspnoea score, priority of surgery, extent of surgery, malignant diagnosis and a comorbidity score)
Question No. 10
Q: How are tests of pulmonary function used to help determine suitability for lung resection surgery?
Answer No. 10
- Important in determining risk of:
- Operative mortality
- Postoperative complications
- Postoperative dyspnoea and unacceptable quality of life
- Assessment includes the use:
- Routine lung function tests:
- Spirometry values (FEV1 / FVC)
- Diffusing capacity for carbon monoxide (TLCO)
- Calculated postoperative predicted values using ventilation/perfusion scans or CT evaluation
- Functional assessments (CPET or shuttle walk test)
- Routine lung function tests:
- In changes from previous guidance, specific cut-offs are no longer recommended but used to risk-stratify patients for shared decision making
Question No. 11
Q: Which values of pulmonary function are used to determine risk associated with lung resection surgery?
Answer No. 11
Question No. 12
Q: What are your anaesthetic goals for lung resection surgery?
Answer No. 12
- Lung isolation to provide optimal surgical field
- Minimisation of acute lung injury during one-lung ventilation
- Safe positioning and careful management of pressure points
- Multimodal analgesia to facilitate postoperative breathing and physiotherapy
- Restrictive fluid therapy and support of haemodynamics
Question No. 13
Q: Describe your possible airway management options for this case? How can you achieve lung isolation?
Answer No. 13
Airway Management
- Usually requires lung isolation with either:
- Double lumen tube (most surgeries performed on L sided tube unless chance of left-sided pneumonectomy in which case R sided tube necessitated
- Single lumen tube and bronchial blocker
- Wedge resection can be performed in selected circumstances with spontaneously breathing patient using a supraglottic airway device
Question No. 14
Q: What are your considerations for intraoperative conduct of patients undergoing lung resection surgery?
Answer No. 14
Monitoring
- Lines usually placed on site of surgery where possible to allow easier access
- Ensure wide-bore peripheral access
- Arterial line usually used for blood pressure monitoring and arterial sampling intraoperatively
- Central line may be recommended on a case by case basis for vasopressor infusions given goal of limited fluid therapy, particularly for larger resections such as pneumonectomy
- Catheter and temperature probe essential
Positioning
- Left or right decubitus position with a table break
- Requires fastidious checking of eye protection, pressure points, and neck position
- Tube position should be rechecked with bronchoscopy after positioning
- Compressions stockings and intermittent pneumatic calf compression devices should be used for DVT prophylaxis
Conduct
- Rigid bronchoscope may be performed prior to pneumonectomy
- Requires isolation and one-lung ventilation for surgical access
- Ventilation should be performed to minimise the risk of lung injury:
- Low tidal volumes based on ideal body weight
- Relatively high PEEP
- Low driving pressures
- Avoidance of hyperoxia
Fluids & Haemodynamics
- Fluids should be restricted whilst avoiding hypovolaemia:
- Excess fluid independent risk factor for postoperative pulmonary oedema
- No clear evidence for benefits of goal directed fluid therapy in lung resection surgery
- In the event of hypotension:
- Haemorrhage must be excluded
- Hypotension secondary to epidural infusion should be treated with vasoactive drugs
Analgesia
- Regional anaesthesia useful for intraoperative and postoperative analgesia:
- Single shot:
- Paravertebral block (anaesthetist or surgeon)
- Intercostal blocks
- Erector spinae plane block
- Serratus anterior block
- Retrolaminar block
- Intrapleural analgesia (via drain)
- Continuous:
- Paravertebral infusion
- Epidural infusion
Intrapleural Infusion
- Single shot:
Question No. 15
Q: What are your postoperative management considerations for patients undergoing lung resection surgery?
Answer No. 15
Location & Review
- Traditionally managed in a high dependency environment
- Immediate management on specialist thoracic ward increasingly recognised as safe for low-risk patients
Monitoring & Investigations
- Close monitoring required to allow early recognition of complications
Supportive Care
- Fluids should be restricted whilst avoiding hypovolaemia:
- Excess fluid independent risk factor for post-operative pulmonary oedema
- Fluid balance within the first 24 h should not exceed 20 ml/kg
- Fluid rate often limited to previous hour's urine output plus 20 ml in the immediate postoperative period
- Ongoing analgesia to allow effective cough and secretion clearance:
- Opioid PCA
- Epidural or paravertebral catheters
- Adjunctive analgesics
- Early and intensive physiotherapy to promote secretion clearance and prevent atelectasis
Question No. 16
Q: What are the complications that can occur following lung resection surgery?
Answer No. 16
Pulmonary
- Pulmonary oedema (9%)
- Post-pneumonectomy syndrome
- Orthodeoxia–platypnoea syndrome
- Lobar torsion (<0.5%)
- Pneumonia
- Atelectasis
- Haemorrhage
- Chronic respiratory failure
Pleural
- Prolonged air leak and persistent pleural space
- Bronchopleural fistula
- Empyema
- Chylothorax
Cardiovascular
- Arrhythmias (AF most common)
- Thromboembolic disease
Other
- Wound infection
- Phrenic nerve injury
- Recurrent laryngeal nerve injury
- Chronic pain
- Death (2%)



