Time: 0 second
SOE 546: Aortic Stenosis
SOE Format:
- Please answer the following questions on the given topic
- The case will be displayed with each question followed by an answer, allowing you to review your given response
- A timer is available for use to determine the given time period
Introduction
A 70-year-old female patient is scheduled for hemiarthroplasty for a fractured neck of femur following a fall. Clinical examination during pre-operative assessment reveals a systolic murmur. You suspect aortic stenosis…
Question No. 2
Q: What are the causes of aortic stenosis?
Answer No. 2
Type
Type
Recommendation
Primary
Congenital
- Bicuspid valve (2% prevalence - typically presents 4th to 6th decade)
- Congenital subaortic membrane
- Other congenital heart disease (e.g. supravalvular stenosis)
Primary
Acquired
- Degenerative (senile) calcification - most common in the UK
- Rheumatic heart disease (usually associated with mitral valve disease)
- Systemic Lupus Erythematosus (SLE)
- Paget's disease
- Radiation
- Drugs
Question No. 3
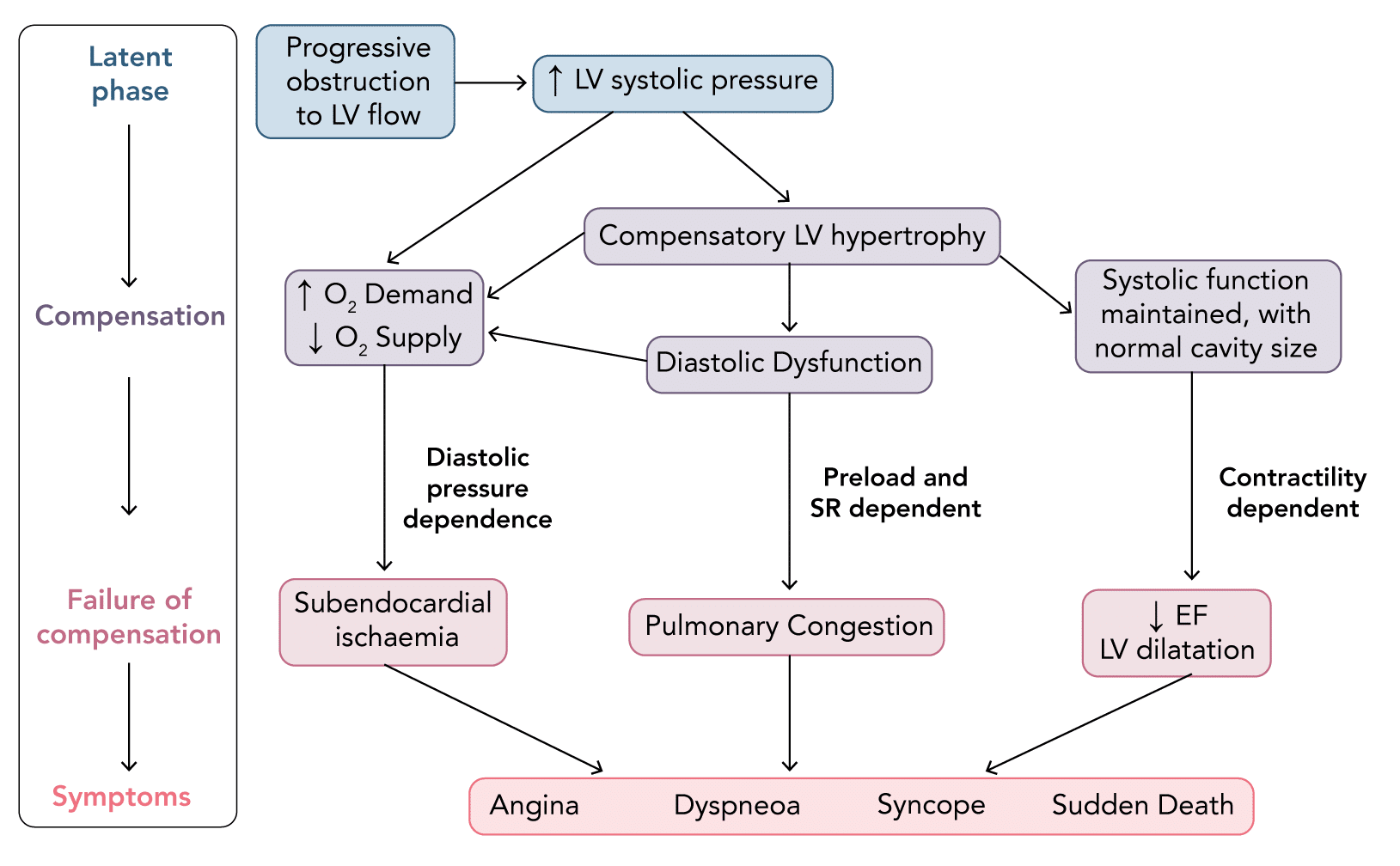
Q: How does it present? What are the symptoms and signs?
Answer No. 3
Symptoms
Classic triad of symptoms:
- Angina
- Can occur with normal coronary arteries
- Caused by increased myocardial oxygen demand due to LV hypertrophyvCompounded by reduced myocardial oxygen supply due to LV hypertrophy distorting flow and coronary calcification
- Syncope
- Occurs during exercise
- Likely due to fixed cardiac output state failing to meet increased demands leading to a drop in cerebral perfusion
- Dyspnoea
- High diastolic pressure leads to pulmonary congestion
- Usually occurs late in disease
Signs
Heart Sounds
- Ejection systolic murmur:
- Harsh, crescendo-decrescendo in nature
- Loudest over the aortic area (second right intercostal space)
- Exacerbated by asking the patient to lean forward and taking a deep breath in.
- May radiate to the carotids.
- May lessen in intensity as the severity increases due to reduced cardiac output
- Ejection click preceding murmur
- Soft or absent S2
Other
- Slow rising pulse
- Low blood pressure and narrow pulse pressure
- Heaving apex beat
- Thrill:
- Precordial
- Carotid
- Inspiratory crepitations (if pulmonary oedema)
Question No. 5
Q: Are you worried about her symptoms?
Answer No. 5
- Yes, the presence of symptoms suggests severe disease with significant haemodynamic obstruction to flow
Question No. 8
Q: How can the severity of aortic stenosis be graded by echo?
Answer No. 8
Grade
Peak gradient
Valve Area
Maximal Aortic Velocity
Mild
<30 mmHg
>1.5 cm2
<3.0 m/s
Moderate
30–50 mmHg
1.0–1.5 cm2
3.0-4.0 m/s
Severe
(Associated with significant haemodynamic compromise)
>50 mmHg
0.6 -1.0 cm2
>4.0 m/s
Critical
>70 mmHg
<0.6 cm2
>4.0 m/s
Question No. 9
Q: Describe your specific haemodynamic goals for the perioperative period?
Answer No. 9
Parameter
Goal
Comment
Preload
↑
- LV hypertrophied and compliance is poor
- Optimize preload to enable adequate filling of the LV (guided by cardiac output monitoring)
- Vasodilators (particularly venodilators such as GTN) should be avoided
Rate & Rhythm
↓
- Avoid tachycardia (Aim 50-70)
- Reduces diastolic filling time
- Reduces the time for coronary perfusion, therefore worsening ischaemia
- Increases oxygen demand
- Avoid excessive bradycardia
- This results in a reduced cardiac output as the stiff ventricle cannot increase the stroke volume to compensate.
- The increase in ventricular filling due to longer diastole also increases ventricular wall tension further reducing coronary perfusion.
Rhythm
Sinus
- Maintain sinus rhythm - vital
- Atrial contraction is important for LV filling
- Up to 40 % of filling in diastole is due to atrial contraction (normally only 15–20 %)
- AF and nodal rhythms are therefore poorly tolerated in these patients
- Arrhythmias need aggressive treatment
Contractility
Maintain
- Maintain myocardial contractility:
- Avoid B-blockers or myocardial ischaemia
- Increasing myocardial drive does not improve cardiac output and can precipitate ischaemia through increased oxygen consumption
Afterload
↑
- Avoiding hypotension is critical - maintain a high-normal diastolic
- Diastolic pressure must be maintained ensure filling of coronary arteries - require larger than usual due to hypertrophied LV
- Any hypotension needs to be treated early to avoid spiral of further reductions in coronary perfusion, causing myocardial depression and potentially leading to cardiac arrest
- CPR is generally ineffective in these patients unless internal massage can be performed
- Afterload essentially fixed below a certain limit due to valvular obstruction:
- Reducing SVR has no impact on ejection of blood from the LV, as the obstruction to flow is due to the stenosed valve leading to a fixed cardiac output
Question No. 10
Q: If the patient requests spinal anaesthesia what would you do?
Answer No. 10
- Classically neuraxial anaesthesia is avoided in severe aortic stenosis:
- Causes reduction in SVR and thus systemic hypotension
- Fixed obstruction impedes compensatory increase in cardiac output
- Can result in spiral of decreased coronary perfusion, ischaemia, further hypotension and death
- Continuous spinal or combined spinal epidural anaesthetic techniques may be used in patients with aortic stenosis
- Allow slow titrated onset of anaesthesia with administration of drugs to maintain blood pressure
- Risks of neuroaxial anaesthesia must be clearly explained to the patient
Question No. 12
Q: Describe your specific postoperative management considerations for a patient with severe aortic stenosis?
Answer No. 12
Location & Review
- HDU / ICU for ongoing BP monitoring:
- NCEPOD recommends admission for valve area <1cm2
- Should be strongly considered if reduced systolic function
Monitoring & Investigations
- Monitor for renal dysfunction
Analgesia
- Avoid NSAIDS - high risk of renal dysfunction
- Ensure optimum analgesia to avoid tachycardia
- Regional anaesthesia may be beneficial
Supportive Care
- Continue haemodynamic aims
- May require vasopressor infusions and ongoing invasive arterial BP monitoring to maintain haemodynamic stability
- Ensure meticulous attention to appropriate intravascular filling