Time: 0 second
SOE 558: Anatomy for Tracheostomy Insertion
Introduction
You review a man on the intensive care ward round who has been intubated for 3 weeks. He was admitted with a community-acquired pneumonia and has been difficult to wean from mechanical ventilation. You suggest the insertion of a percutaneous tracheostomy to aid weaning from the ventilator…
Question No. 2
Q: What is the preferred site of insertion for percutaneous tracheostomy and why?
Answer No. 2
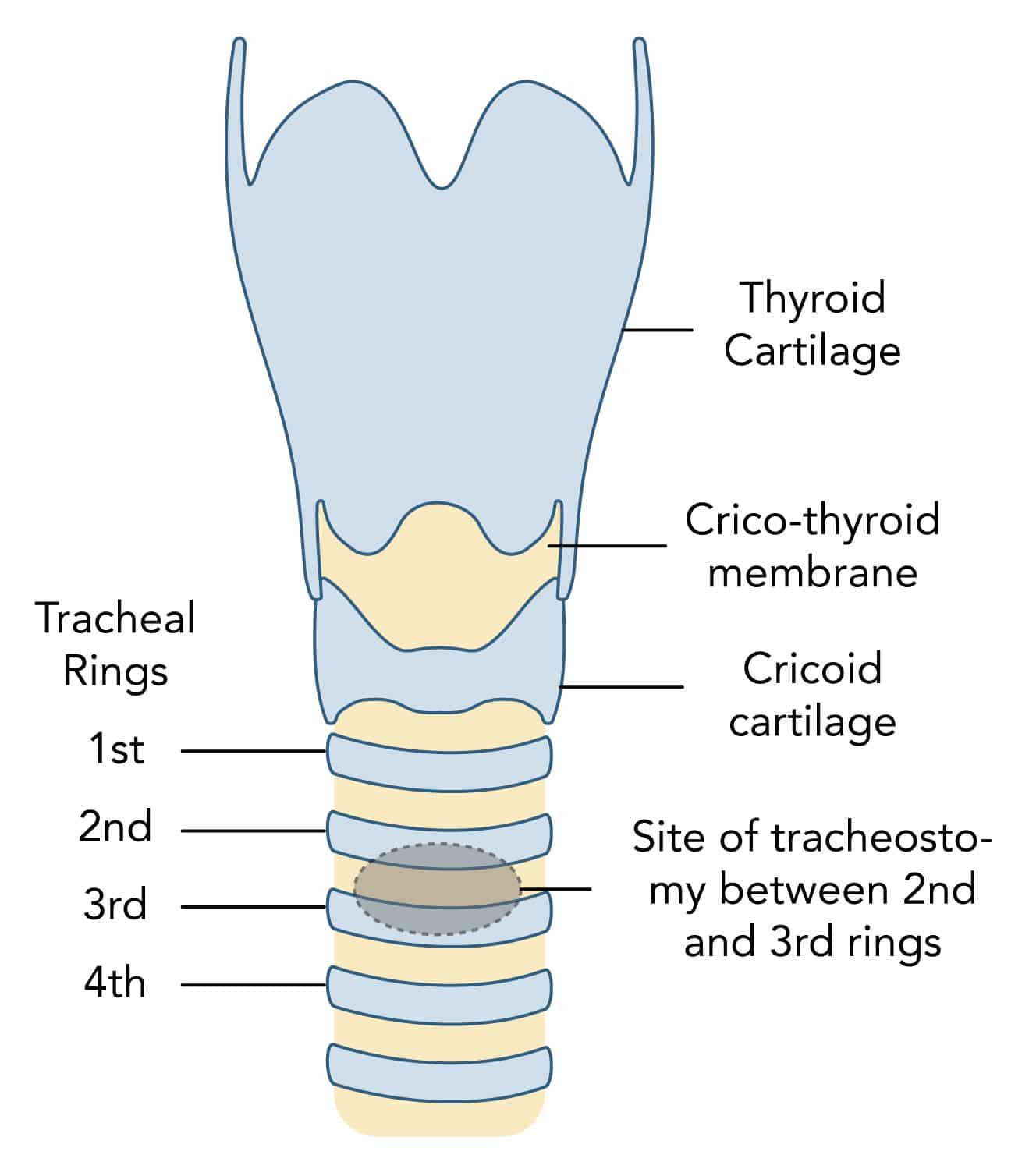
- Preferred site of tracheostomy is between the 2nd and 3rd tracheal rings in the midline
- Tracheostomy above this site:
- Can lead to damage to the cricoid cartilage and first tracheal ring
- Results in increased risk of subglottic stenosis which is difficult to treat
- Tracheostomy below this site:
- Can lead to damage to the thyroid and great vessels at the root of the neck
- Results in increased risk of significant bleeding
Question No. 4
Q: What is the structure and course of the trachea?
Answer No. 4
- Tube of cartilage with a membranous lining continuous with the larynx
- Composed of 16–20 C-shaped cartilaginous rings
- Trachealis muscle completes the posterior wall
- Around 10-12 cm in length
- Extends down from cricoid at C6
- Terminates at carina at T5-
- Moves anteriorly to posteriorly from the cricoid distally
- Enters the chest behind the sternal notch
Question No. 5
Q: Which structures are in close relationship to the trachea?
Answer No. 5
Anterior Relations
- Skin and fascia
- Isthmus of thyroid
- Sternothyroid and sternohyoid muscles
- Manurbrium sternum
- Thymus gland
Lateral Relations
- Lobes of thyroid
- Carotid sheath
- Lungs and pleura
- Arch of aorta, brachiocephalic and subclavian arteries
Posterior Relations
- Oesophagus
- Recurrent laryngeal nerve
Question No. 6
Q: Which vessels are at risk of damage during tracheostomy?
Answer No. 6
- Anterior jugular veins:
- Run vertically close to the midline
- Thyroid ima artery :
- Ima is 'lowest' in Latin
- Anatomical variant in 3–10% of the population
- More common British Asian populations
- Arises mainly from the brachiocephalic trunk and ascends along the front of the trachea
- Inferior thyroid veins
- Other vessels more lateral: internal jugular vein, carotid artery, external jugular vein
Question No. 7
Q: What are the indications for a tracheostomy?
Answer No. 7
Overcome Upper Airway Obstruction (Actual or Potential)
- Tumour
- Bilateral recurrent laryngeal paresis
- Oral / facial trauma
- Infection in oral cavity, pharynx or larynx
- Burns
- Following certain head and neck surgery
Facilitate Airway Protection and Secretion Management
- Laryngeal incompetence due to critical illness, polyneuropathy, or bulbar dysfunction
- Neurological disease
- Traumatic brain injury
Facilitate Weaning from Mechanical Ventilation
- Any reversible condition requiring ventilatory support
Provide Lifelong Ventilation
- High C-spine injury
Question No. 8
Q: Is there any evidence to suggest early tracheostomy is superior to late tracheostomy to aid weaning from ventilation?
Answer No. 8
- No high-quality studies have definitively answered the question of whether routine, early tracheostomy improves clinical outcomes:
- Studies are difficult to design
- Doctors are poor at predicting which patients may undergo successful extubation within the next few days, thereby avoiding unnecessary tracheostomy
- Accumulated evidence and expert opinion suggest early tracheostomy does not improve survival or even shorten hospital stay
- The largest trial to explore the question is the TRACMAN trial:
Population
Intervention
Conclusion
- Intubated and ventilated patients expected to require at least seven further days of ventilation
- Excluded those with potential indications for early tracheostomy (airway obstruction, neurological illness, TBI)
- Early (within four days of admission) vs. late (on/after day 10) tracheostomy
- Primary outcome 30-day mortality
- No difference in mortality at any point over the two-year follow-up
Early group: - Non-significant trend towards shorter duration of mechanical ventilation
- Significantly fewer days of sedation administration
Late group: - Only 43% of the patients in the late group went on to receive a tracheostomy (many not intubated)
- 6.3% complication rate for the tracheostomies that were performed
- Eight RCTs with a total of 1,977 participants
- Early tracheostomy (two to 10 days after intubation) vs. late tracheostomy (> 10 days after intubation) for critically ill adult patients
- Results from seven RCTs (n = 1903) showed lower mortality rates in the early as compared with the late tracheostomy group (risk ratio (RR) 0.83, P value 0.03)
- However due to low quality evidence review concluded results "no more than suggestive of the superiority of early over late tracheostomy"
Question No. 9
Q: What are the advantages of a tracheostomy?
Answer No. 9
- Reduction in laryngeal and vocal cord trauma
- Prolonged intubation associated with injury such as pressure necrosis and mucosal abrasions
- Reduced sedation requirement (better tolerated than ETT)
- Facilitation of gradual weaning from mechanical ventilation:
- Reduced work of breathing
- Reduced resistance and dead space
- Improved oral hygiene
- Allows rehabilitation:
- Improved mobility, speaking, oral intake
- Improved patient communication (written or spoken)
- Improved patient comfort
- Reduced LOS in ICU
- Reduced nursing care required
Question No. 10
Q: What are the different techniques for front of neck airway access?
Answer No. 10
Surgical Tracheostomy
- An open surgical procedure that allows insertion of a tracheostomy tube into the trachea between cartilaginous rings.
Percutaneous Dilatational Tracheostomy
- Refers to various procedures that have in common either a modified Seldinger technique for placing a modified tracheostomy tube or a forceps technique to cannulate and dilate tracheal tissue between cartilaginous rings
- Used for over 90% of ICU tracheostomies with over two-thirds of all tracheostomy procedures are now performed by intensivists in ICUs rather than by surgeons
Cricothyroidotomy
- Technique for placement of an airway into the trachea through the cricothyroid space
- Can be performed as a surgical procedure through an incision, as a percutaneous procedure by a Seldinger technique, or as a needle cricothyroidotomy for emergency airway access.
Mini Tracheostomy
- Allows percutaneous placement of a 7F cannula through the tracheal rings to allow suctioning for patients with difficulty clearing airway secretions
Question No. 11
Q: What are the advantages and disadvantages of surgical / percutaneous tracheostomies?
Answer No. 11
Percutaneous
Surgical
Advantages
- Relatively quick in experienced hands
- Avoids need for transfer of unstable patients
- Does not require involvement of surgeons
- Cheaper
- Smaller scar
- Tighter stoma that decreases stomal bleeding and provides better fit
- Can be performed when percutaneous contraindicated:
- Short or thick neck, obese
- Coagulopathy
- Unstable spine
- Previous neck / thyroid surgery
- Abnormal vessels
- Resources available to control bleeding
- Potentially easier management in event of early tube dislodgment or tube exchange:
- Stoma stitched open
- May have stay sutures to elevate the trachea
Disadvantages
- Suboptimal conditions for management of bleeding, especially if major vessel injured
- Blind techniques can be incorrectly positioned
- Tracheal ring fracture can occur
- Late tracheal stenosis (as per surgical tracheostomy)
- Lack of surgical dissection can increase risk of vascular or thyroid injury
- Potentially more difficult management in event of early tube dislodgment or tube exchange:
- Tissues will tend to ‘spring’ closed when tube removed in first 7–10 days
- Requires operating theatre leading to delays in insertion
- Requires patient transfer
- More expensive
Question No. 12
Q: What are the contraindications to tracheostomy?
Answer No. 12
Absolute Contraindications
- Patient Refusal
- Unstable fractures of the cervical spine
- Severe local infection of the anterior neck
- Uncontrollable coagulopathy
Relative Contraindications
- Lack of need:
- Unlikely to survive >48 hours
- Unlikely to require >2 weeks ventilation
- Controlled local infection
- Coagulopathy:
- PT or APTT >1.5
- Platelets <50
- High PEEP (>10) or FiO2 (>0.6) requirements
- Difficult anatomy (contraindication to percutaneous tracheostomy, surgical tracheostomy advised):
- Abnormal or prominent vasculature at insertion site
- Morbid obesity
- Short thick neck
- Reduced neck extension
- Excessive goiter
- Tracheal deviation
- Previous radiotherapy
- Proximity to extensive burns or surgical wounds
- Elevated intracranial pressure
- Haemodynamic instability
Question No. 13
Q: What are the complications of percutaneous tracheostomy?
Answer No. 13
Immediate (During Insertion)
- Arrest and Death (1/600)
- Haemorrhage (minor or severe) - 4.8%
- Misplacement (pre-tracheal tissues or to main bronchus)
- Hypoxia
- Injury to local structures:
- Pneumothorax and surgical emphysema
- Oesophageal perforation
- Vascular injury
- Thyroid injury
- Posterior tracheal wall injury
- Laryngeal nerve damage
- Tracheal ring fracture
- Air embolism
- Equipment issues:
- Incorrect tube / size
- Equipment malfunction
Delayed (Post Insertion)
- Tube blockage with secretions (may be sudden or gradual)
- Tube migration to pre-tracheal space
- Accidental decannulation
- Infection:
- Stoma site
- Bronchial tree
- VAP
- Erosion related:
- Tracheal ulceration or necrosis
- Tracheo-oesophageal fistula formation
- Tracheo-innominate fistula
Late (Post Decannulation)
- Tracheal injury / dysfunction:
- Tracheal stenosis at the cuff site
- Tracheomalacia
- Vocal cord dysfunction
- Persistent sinus at the tracheostomy site
- Granulomata of the trachea
- Tracheo-innominate fistula
- Psychological impact related to stoma