Time: 0 second
SOE 037: Renal Replacement Therapy 2
Introduction
You are called to see a 68-year-old man is 2 days post-operative following a femoral endarterectomy for an acutely ischaemic limb. He has developed rhabdomyolysis with morning bloods demonstrating an elevated creatine kinase (23,482 U) and an elevated creatinine (349 Umol/L)…
Question No. 3
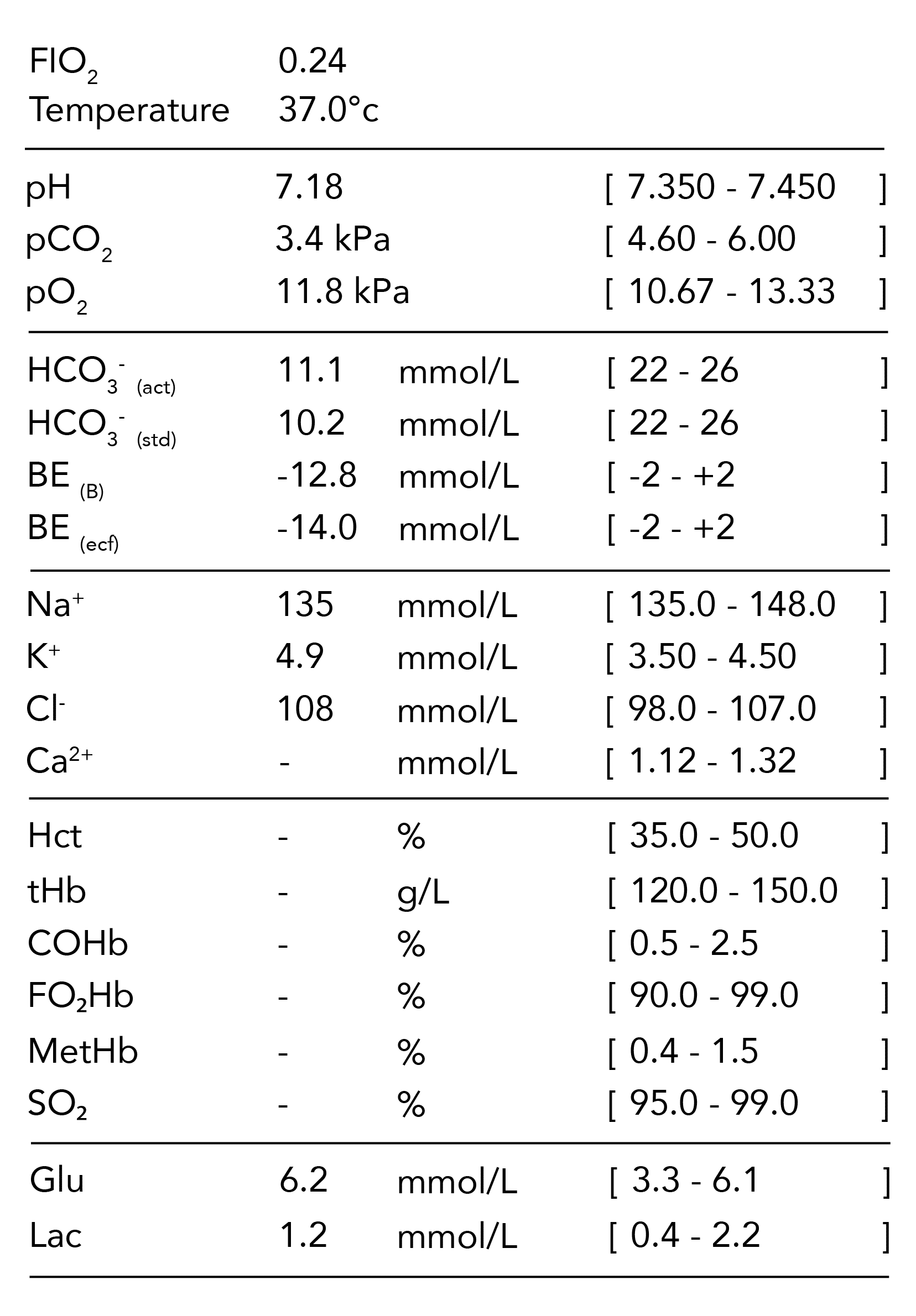
Q: Can you describe the findings from the blood gas?
Answer No. 3
Summary
Summary
Summary
There is a profound high anion-gap metabolic acidosis with partial respiratory compensation
There is a profound high anion-gap metabolic acidosis with partial respiratory compensation
There is a profound high anion-gap metabolic acidosis with partial respiratory compensation
Description
Description
Description
Acid-Base Status
1. Primary Disorder
- The primary disorder is a metabolic acidosis with a BE of -14.
Acid-Base Status
2. Compensation & Secondary Disorder
- There is partial respiratory compensation
- The measured (3.4 kPa) and expected (3.5 kPa) are similar so a secondary respiratory disorder is not suggested
Acid-Base Status
3. Assessment of Metabolic Acidosis
- The anion gap is 24 mmol/L indicating the presence of a HAGMA
- The delta ratio is 0.85 indicating an isolated HAGMA
Acid-Base Status
4. Assessment of HAGMA
- Osmolarities not provided
Acid-Base Status
5. Assessment of NAGMA
- Not applicable
Oxygen Status
6. Assessment of oxygenation
- There is slight impairment of oxygenation with P/F ratio of 46.25
Oxygen Status
7. Assessment of oxygen carriage
- Co-oximetry values not provided
Question No. 4
Q: Other than metabolic acidosis what are the indications for renal replacement therapy?
Answer No. 4
Renal Indications
Emergency Indications
- Metabolic
- ↑ K+ (>6.5 mmol/L)
- ↑ urea (>40 mmol/L)
- Uraemia with symptoms:
- Pericarditis
- Encephalopathy
- Refractory pulmonary oedema
- Metabolic Acidaemia due to renal failure (pH<7.15)
- Oligo-anuria(<200ml/24 hours)
Non-Emergency Indications
- Acheivement of homeostasis in AKI unresponsive to conservative management
- Acid-base balance
- Solutes
- Fluid
Non-Renal Indications
- Removal of dialysable toxins
- Removal of contrast agent (Less relevant with newer contrast agents)
- Clearance of cytokines to decrease severity of sepsis (controversial)
- Control of body temperature (an extracorporeal circuit can help control hypo or hyperthermia which is resistant to other methods of control)
- Control of otherwise uncontrollable electrolytes:
- ↑ Ca+ refractory to pamidronate
- Sodium abnormalities resistant to treatment
Question No. 6
Q: How does the circuit differ for haemodialysis and haemofiltration?
Answer No. 6
Haemodialysis
Haemofiltration
Haemodiafiltration
SCUF
Question No. 7
Q: What variables are controlled through the circuit that influence its function?
Answer No. 7
Blood Flow Rate
Blood Flow Rate
Qb
- The rate of blood flow from the patient towards the filter
- Blood flow rates are typically slower than in intermittent dialysis, ranging from 150-200mL/min
Ultrafiltrate Rate
Ultrafiltrate Rate
Quf
- The rate at which ultrafiltrate is produced by hydrostatic pressure across the membrane during convective therapies
- It is influenced by the blood flow rate and the filtration fraction
Dialysate Flow Rate
Dialysate Flow Rate
Qd
- The flow rate of dialysis fluid in dialytic therapies
- Standard flow rates range from 8-50 mL/min
Effluent Rate
(Dose)
(Dose)
Effluent Rate
(Dose)
(Dose)
Qef
- The effluent flow rate is the equivalent to ultrafiltration rate Quf in continuous haemofiltration, Qd in continuous haemodialysis, and both Quf & Qd in continuous hemodiafiltration
- It is analogous to the ‘dose’ in continuous therapies
- Dosing is weight-based and is typically prescribed at a dose ranging from 20 mL/kg/hr to 35 mL/kg/hr
Substitution Fluid Rate
Substitution Fluid Rate
Qs
- Techniques in which produce a volume of ultrafiltrate require replacement of this fluid with a substitute fluid to prevent significant loss of volume.
- The rate of substitution fluid describes the rate at which this replacement fluid is added to the plasma
Net Ultrafiltrate Rate
Net Ultrafiltrate Rate
Qnet
- Represents the overall rate of fluid removal
- It is the difference between the total effluent removed (Qef) minus the volume of replacement therapy
- The fluid removal rate can be tailored by the machine to meet the total removal goal of the patient
Question No. 8
Q: What determines the clearance in CRRT? How is the effluent rate determined?
Answer No. 8
- Clearance describes the volume of blood that is cleared of a substance per unit of time
- The determinant of clearance in CRRT depends upon the mechanisms that are being utilised
- In continuous haemofiltration:
- A volume of ultrafiltrate is produced following the passage of the pressurised plasma over the membrane
- Clearance is of a solute determined by the:
- Rate at which ultrafiltrate is produced (Quf)
- Sieving coefficient of the filter membranes (determined by the ratio of solute concentrations in the ultrafiltrate)
- Most small molecules have a sieving coefficient of 1, meaning they pass freely through the membrane (though this is less true of middle molecules)
- Therefore, the clearance is analogous to the ultrafiltrate production rate (Quf)
- In continuous haemodialysis:
- The concentration gradient across the membrane determines clearance
- The gradient is affected by the dialysate flow rate (Qd) and the blood flow rate (Qb)
- Qd is much slower than Qb, and the dialysate becomes fully saturated.
- Therefore, the dialysate rate (Qd) becomes the rate-limiting factor for solute removal and is analogous to clearance
- Overall consequently, clearance is equivalent to the combination of the ultrafiltration rate (Quf) and dialysate (Qd), which is termed the effluent rate (Qef)
- This is often discussed in terms of the ‘dose’ of a continuous replacement therapy which is given
- In continuous haemofiltration:
- In ultrafiltration, the effluent rate is determined by the flow of plasma into the membrane and the fraction of this which is filtered out as effluent (known as the filtration fraction)
- To maintain a constant effluent rate:
- At low blood flows a large filtration fraction is required
- At high flows, a small filtration fraction can be used
- The renal replacement circuits have inbuilt algorithms to deliver a desired effluent flow rate based upon the blood flow from the patient
Question No. 9
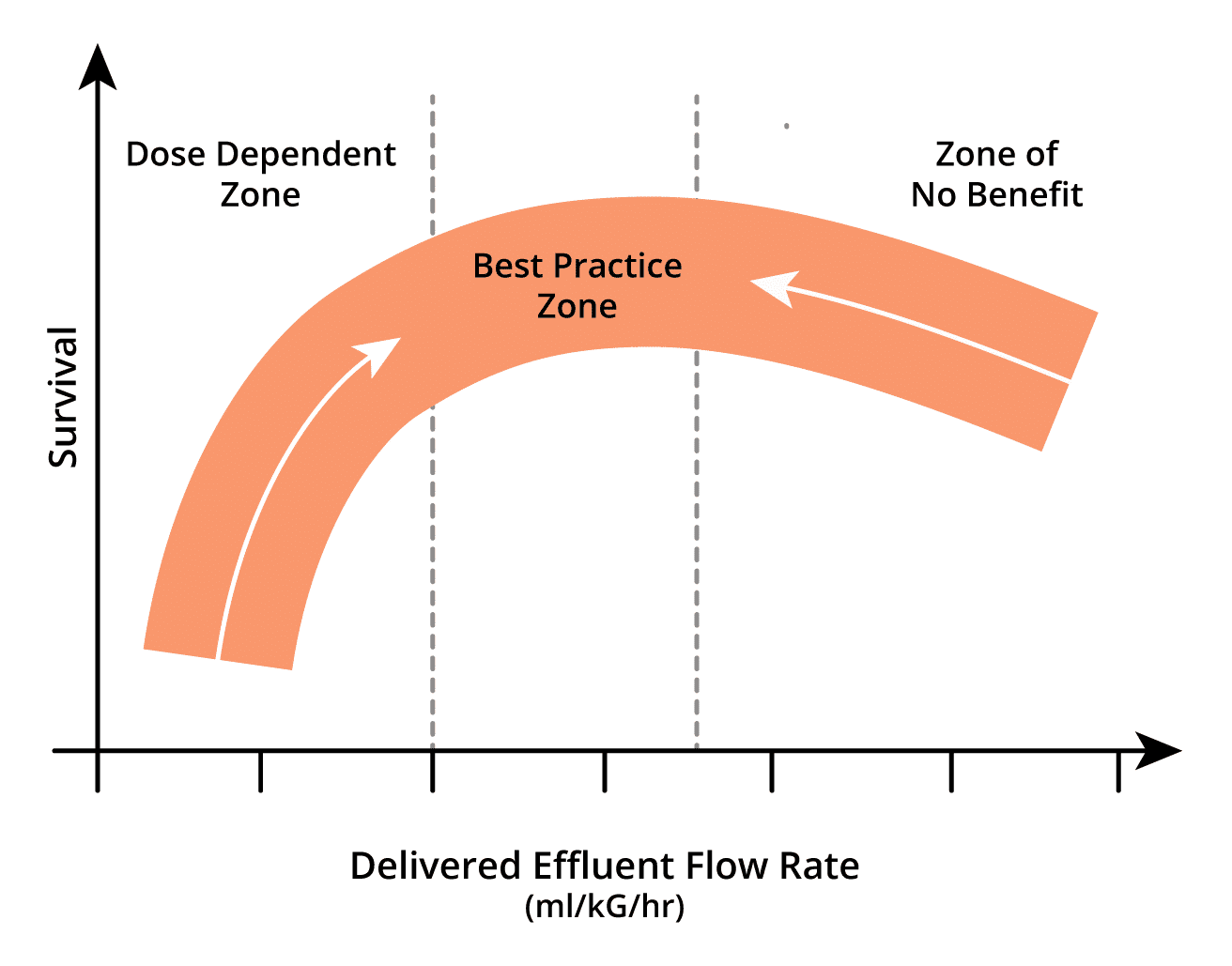
Q: What is the optimal dose of CRRT in AKI?
Answer No. 9
- Adequate clearance, and how this influences outcome is not clear:
-
- Current research suggests that a rate of 20-25ml/kg is adequate
- Higher rates of clearance (35-40ml/kg) confer no benefit
- Higher rates may need to be prescribed to ensure minimum desired clearance is met
- High volume hemofiltration may be of benefit in:
- Rhabdomyolysis
- Clearance of ammonia and lactate
- Pancreatitis (experimental)
- Clearance of cytokines (experimental)
Question No. 10
Q: What evidence exists to determine the optimum ‘dose’ of CRRT?
Answer No. 10
Intervention
Population
Conclusion
- Early vs. Late initiation of RRT
- Early: Within 8 hours of meeting KDIGO stage 2 AKI
- Late: Within 12 hours of meeting KDIGO stage 3 AKI or emergency indication
- 231 patients with AKI and either severe sepsis or requiring catecholamine infusion
- Early group showed significantly lower mortality at 90 days (39.3% vs. 54.7%, p=0.03)
- Early vs. Late initiation of RRT
- Early: Immediately upon meeting KDIGO stage 3 AKI criteria
- Late: If oliguric 72 hours after meeting KDIGO stage 3 AKI criteria or emergency indications
- 620 patients with AKI requiring mechanical ventilation or catecholamine infusion
- No difference in mortality between early and late group (48.5% vs 49.7%, p=0.79)
- In delayed group 49% did not require RRT
- Early vs. Late initiation of RRT
- Early: within 12-hours of meeting failure by RIFLE criteria
- Late: after 48-hours of meeting failure by RIFLE criteria if no renal recovery or emergency indications
- 488 patients with severe AKI and septic shock
- No difference in mortality between early and late group (58% vs 54%, p=0.38)
- In delayed group:
- 38% did not require RRT
- 17% met indications for emergency RRT
Question No. 11
Q: What is difference between prescribed and delivered dose? What dose should be prescribed?
Answer No. 11
- There may be a significant difference between the prescribed ‘dose’ and that which is actually delivered – estimated using clearance equations to be 73% in practice
- Due to a number of factors:
- Treatment downtime due to filter clotting
- Technical problems such as boor blood flow and recirculation
- Reduced filter efficacy over time
- Effects of pre-dilution
- It is recommended that a dose of at least 35 ml/kg/h (post-dilution) is prescribed for CRRT
- This ensures that an adequate dose of CRRT is delivered despite downtimes and other limiting factors
Question No. 12
Q: What is the prognosis of patients requiring RRT in ICU?
Answer No. 12
- Mortality remains high in critically ill patients
- Mortality around – 45-60% in studies
- RRT withheld in around 20% of patients
- Of those that survive to ICU discharge:
- If no chronic renal impairments prior to admission:
- Long-term RRT required in 2-11%
- CKD in 44%
- If chronic renal impairment prior to admission:
- Long-term RRT required in up to 55%
- If no chronic renal impairments prior to admission:
Question No. 13
Q: What are the complications of RRT?
Answer No. 13
Access Related
- Failure to obtain access
- Damage to vessels and surrounding structures
- Risk of venous stenosis
- Haemorrhage
- Infection
- Air Embolism
- Pain
Anticoagulation Related
- Bleeding
- Heparin induced thrombocytopenia
- Hypocalcaemia with citrate
Filtration Related
- Hypotension and haemodynamic instability:
- Common on initiation of renal replacement as the circuit often takes 200-300 ml of blood
- Usually responds to a fluid bolus
- Removal of solutes:
- Electrolyte imbalance
- Trace elements and amino acids
- Therapeutic drugs
- Metabolic abnormalities
- Reaction to filter membrane and anaphylaxis
- Rising lactate:
- Inability to metabolise lactate in the filter fluid to bicarbonate
- Switch to filter fluid with bicarbonate buffer