Time: 0 second
Question No. 2
Q: What are the clinical features that may suggest pulmonary embolism as a cause of a patients deterioration?
Answer No. 2
- Clinical features are non-specific and have been shown to be of limited value in confirming the diagnosis
- Features range from being relatively asymptomatic to significant cardiovascular compromise - they can be difficult to identify in the sedated, mechanically-ventilated patient
- Haemodynamic instability is a rare but important form of clinical presentation, as it indicates central or extensive PE with severely reduced haemodynamic reserve
- Common features include:
Symptoms
- Pleuritic chest pain
- Dyspnea
- Hemoptysis
Signs
- Acute onset of tachypnea
- Hypoxia or increased oxygen requirements
- Tachycardia
- Hypotension
- Unexplained agitation
- Asymmetric leg swelling
- Weaning failure
- Persistent pyrexia without evident source of infection
- Cardiovascular and respiratory examination findings:
- Pleural friction rub
- Small volume arterial pulse
- Raised jugular venous pressure
- Gallop rhythm at the left sternal edge
- Accentuated second heart sound
Question No. 3
Q: How common is pulmonary embolism?
Question No. 4
Q: What is the mortality associated with pulmonary embolism?
Answer No. 4
- Mortality rates range in studies range from 6% - 15%
- In 2004 this equated to 370 000 deaths across Europe
- 34% died suddenly or within a few hours of the acute event
- 59% diagnosed after death
Only 7% who died early were correctly diagnosed with PE before death
Question No. 5
Q: What are the risk factors for VTE in the critically ill?
Answer No. 5
Can be considered according to Virchow’s triad:
Venous Stasis
- Prolonged bed rest
- Prolonged air travel (>8 hours)
- Fracture of lower limbs
- Hip or knee replacement
- Spinal cord replacement
- Varicose veins
Hypercoagulability
- Malignancy (particularly metastatic disease)
- Infection (specifically pneumonia, urinary tract infection, and HIV)
- Specific thrombotic conditions:
- Previous venous thrombosis
- Factor V Leiden mutation
- Protein C or S deficiency
- Hyperhomocysteinemia
- Antithrombin III deficiency
- Antiphospholipid antibodies
- Thrombotic thrombocytopenic purpura (TTP)
- High levels of factor VIII
- Nephrotic syndrome
- Inflammatory bowel disease
- Pregnancy
- Drugs:
- Hormone replacement therapy
- Oral contraceptives
- Tamoxifen
- Chemotherapy
- Heart failure or respiratory failure
- Increasing age
- Obesity
Endothelial Injury
- Major surgical procedures
- Trauma
- Prior venous thrombosis
- Venous catheters
- Smoking
- Hypertension
Question No. 6
Q: How can the severity of PE be classified?
Answer No. 6
- Classification of PE severity has traditionally been based on haemodynamic stability:
Massive
- Cardiovascular compromise with a systolic blood pressure (SBP) <90 mmHg or a drop in systolic pressure of >40 mmHg
Sub-Massive
- No systemic hypotension but evidence of either RV dysfunction or myocardial necrosis
Mild / Non-Massive
- Asymptomatic or with mild symptoms and no evidence of RV dysfunction or cardiovascular compromise
- Newer classifications of severity are based upon early mortality risk (in-hospital or 30-days) using clinical, imaging, and laboratory indicators:
Early Mortality Risk
Early Mortality Risk
Risk Parameters & Scores
Risk Parameters & Scores
Risk Parameters & Scores
Risk Parameters & Scores
Early Mortality Risk
Early Mortality Risk
Shock or hypotension
PESI class III-V
Signs or RV Dysfunction on Imaging
Cardiac Laboratory Biomarkers
High
High
+
(+)
+
(+)
Intermediate
High
-
+
Both positive
Both positive
Intermediate
Low
-
+
Either one (or none) positive
Either one (or none) positive
Low
Low
-
-
-
Assessment optional but negative if assessed
Question No. 7
Q: How is haemodynamic instability defined in the setting of high-risk pulmonary embolism?
Answer No. 7
Cardiac arrest
- Need for cardiopulmonary resuscitation
Obstructive shock
- Systolic BP <90 mmHg or vasopressors required to achieve a BP ≥90 mmHg despite adequate filling status
and - End-organ hypoperfusion (altered mental status; cold, clammy skin; oliguria/anuria; increased serum lactate)
Persistent hypotension
- Systolic BP <90 mmHg or systolic BP drop ≥40 mmHg, lasting longer than 15 min and not caused by new-onset arrhythmia, hypovolaemia, or sepsis
Question No. 9
Q: What are the electrocardiographic (ECG) findings seen in PE?
Answer No. 9
- ECG findings are also variable and neither sensitive or specific
- A normal ECG is seen in up to 18% of cases
- Abnormalities seen include:
- Sinus tachycardia (most common - 44%)
- Atrial arrhythmias (most frequently atrial fibrillation)
- Classic S1Q3T3 (10%)
- Deep S-wave in lead I, Q-wave in III and an inverted T-wave in III
- Complete or incomplete right bundle branch block (15%): rSR’ in V1
- Associated with increased mortality
- Acute right ventricular strain (34%)
- T-wave inversion in the right precordial leads (V1-4) and the inferior leads (II, III, aVF)
Associated with high pulmonary artery pressures
- T-wave inversion in the right precordial leads (V1-4) and the inferior leads (II, III, aVF)
- Right axis deviation (15%):
- May be extreme deviation - between 0 and -90°
- Non-specific ST-segment and T-wave changes:
- ST-elevation and depression
- T-wave inversion
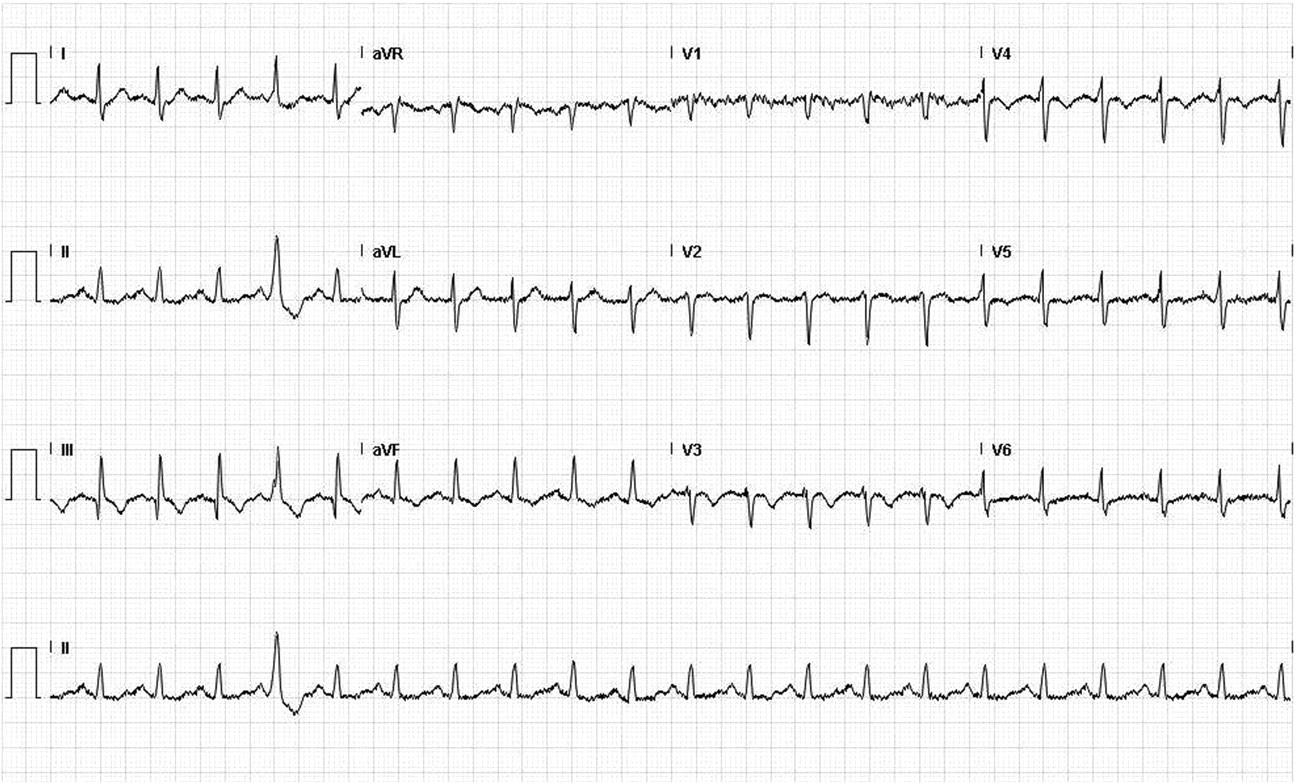
An ECG in pulmonary embolism demonstrates:
- S1Q3T3 pattern - an S wave in lead I, Q wave and an inverted T wave in lead III
- Sinus tachycardia
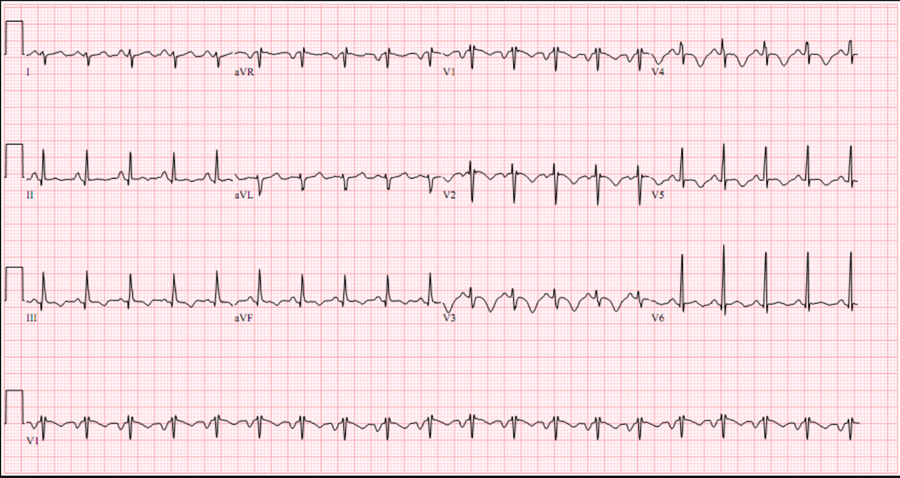
An ECG in pulmonary embolism demonstrates:
- Incomplete or complete RBBB (rSR’ in V1)
- T wave inversion in V1-V3 - mimics anterior ischemia
- Sinus tachycardia

An ECG in pulmonary embolism demonstrates:
- Right axis deviation
- Right bundle branch block (rSR’ in V1)
- Deep T wave inversion in V1-V3
- Sinus tachycardia
Question No. 11
Q: Why do pulmonary emboli cause haemodynamic instability?
Answer No. 11
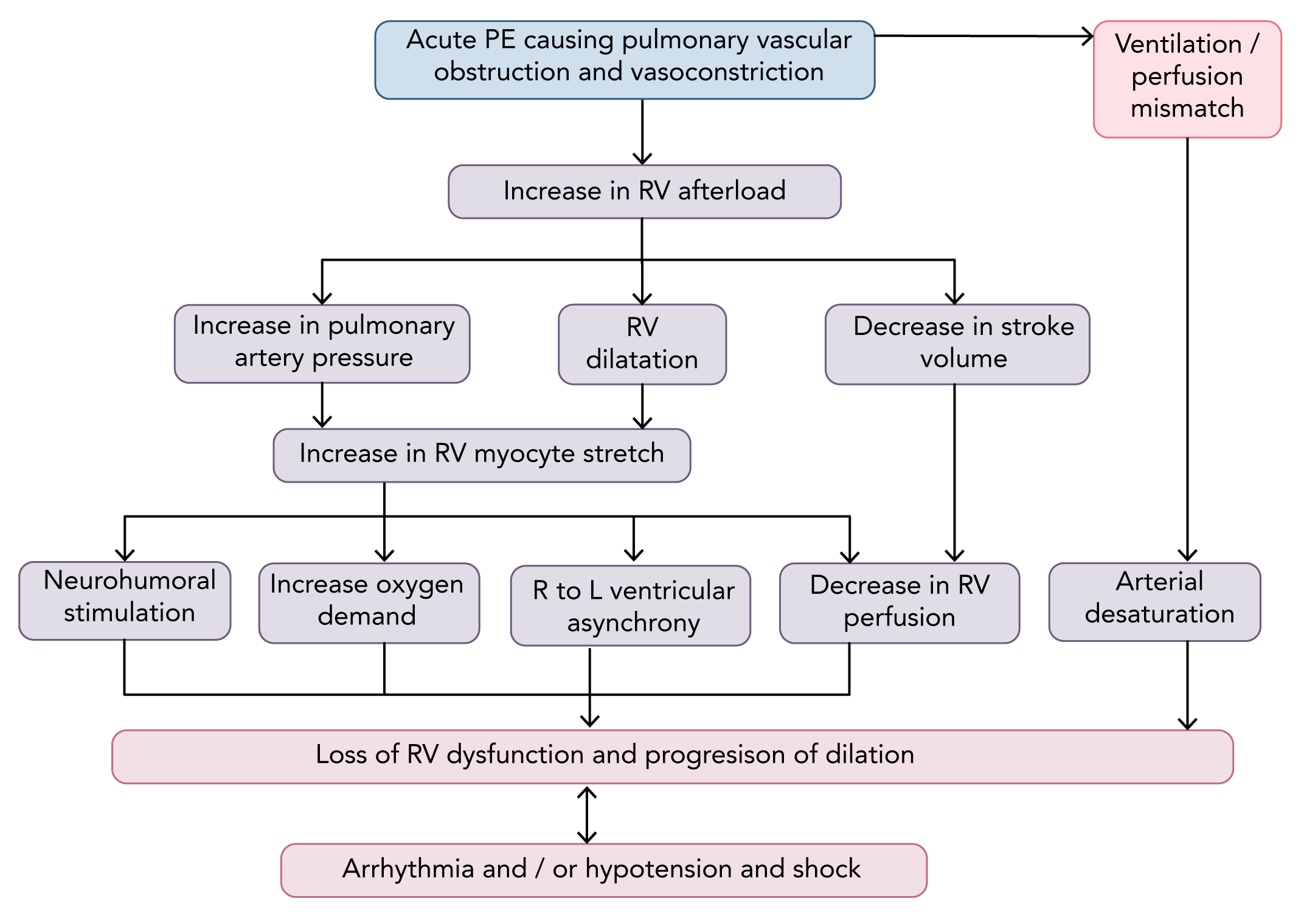
- PE can lead to right ventricular (RV) failure due to acute pressure overload:
- Pulmonary artery pressure (PAP) increases in the presence of obstruction
- Becomes evident if >30-50% of the total cross-sectional occluded by thromboemboli
- Obstruction due to:
- Mechanical obstruction from clot burden
- Vasoconstriction, mediated by the release of thromboxane A2 and serotonin
- Results in increased RV afterload and subsequent dilatation:
- Initial compensation occurs via Frank Starling mechanism with increased myocyte stretch
- Neurohumoral activation leads to inotropic and chronotropic stimulation.
- RV adaptation is limited and is unable to generate a mean PAP >40 mmHg
- Ventricle non-preconditioned and thin-walled
- Enters cycle of progressive RV failure with imbalanced oxygen supply / demand and decreased contractility
- Progressive impact on left ventricle (LV) and systemic circulation:
- Bowing of intraventricular septum impairs LV filling
- Further exacerbated by development of right bundle branch block
- Leads to reduced cardiac output and systemic hypotension
- Exacerbates impaired coronary driving pressure to the overloaded RV and further imbalances myocardial oxygen supply and demand
- May be a secondary inflammatory response due to massive neurohumoral activation
Question No. 12
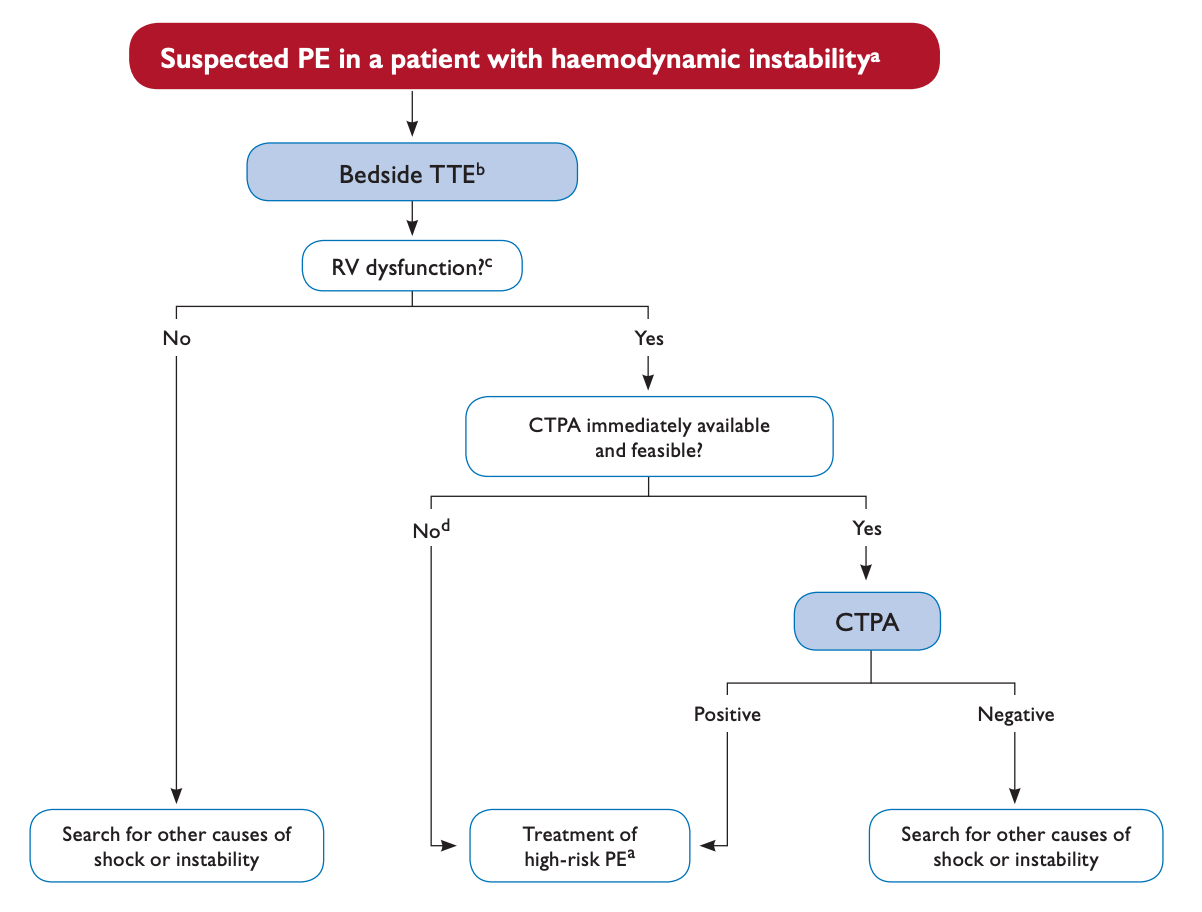
Q: How would your diagnostic strategy change now the patient is demonstrating haemodynamic instability?
Answer No. 12
Question No. 13
Q: What are the echocardiographic findings seen in PE?
Answer No. 13
- Dilatation of the right ventricle
- Impaired right ventricular function
- Flattened intraventricular septum
- Distended inferior vena cava with diminished inspiratory collapsibility
- Tricuspid regurgitation
- Mobile thrombus in the right heart
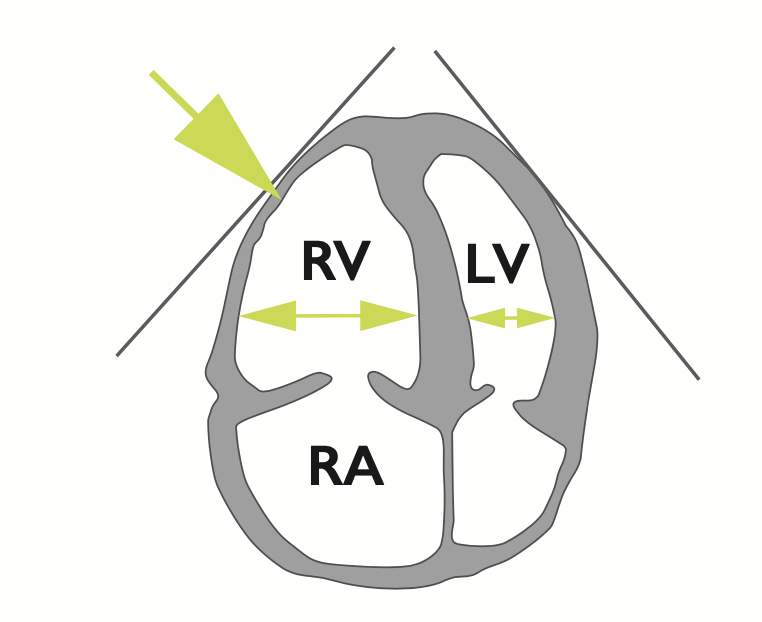
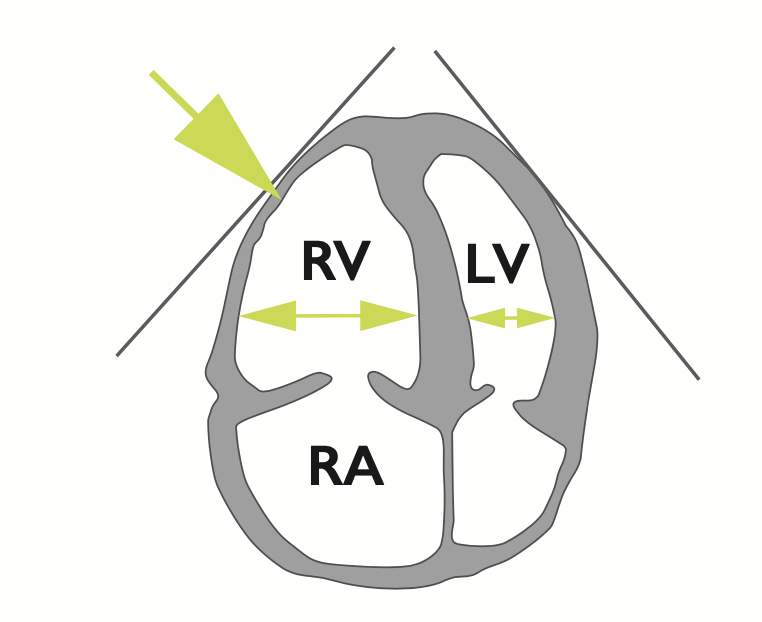
Dilatation of the right ventricle
- Basal RV/LV > 1.0
- RV >4cm at the base in the 40 chamber view

Impaired right ventricular function
- Tricuspid annular plane systolic excursion (TAPSE) <16 mm
- May be evident on visual evaluation
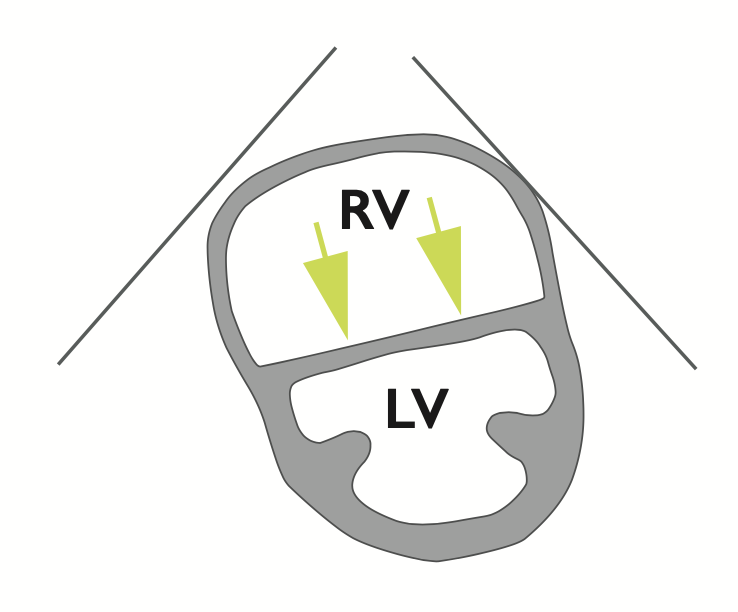
McConnel's sign
- Normokinesia and/or hypokinesia of the apical segment of the RV free wall despite hypokinesia and/or akinesia of the remaining parts of the RV free wall
Flattened intraventricular septum
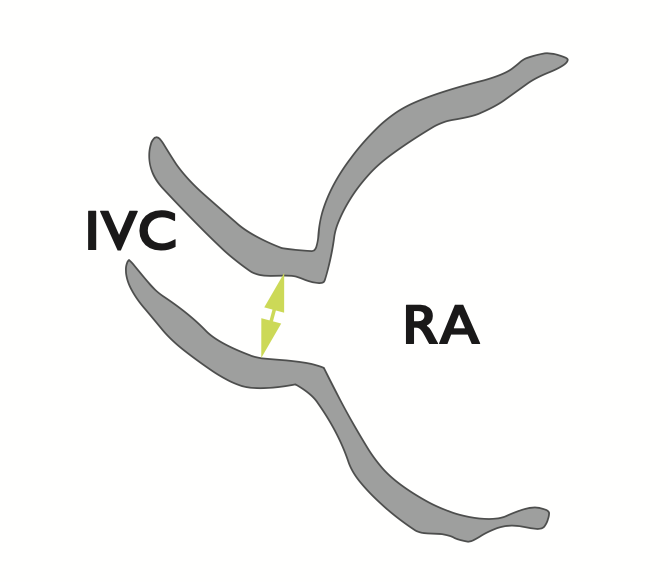
Distended inferior vena cava with diminished inspiratory collapsibility
Tricuspid regurgitation
- Velocity greater than 2.7 m/sec by colour doppler flow imaging
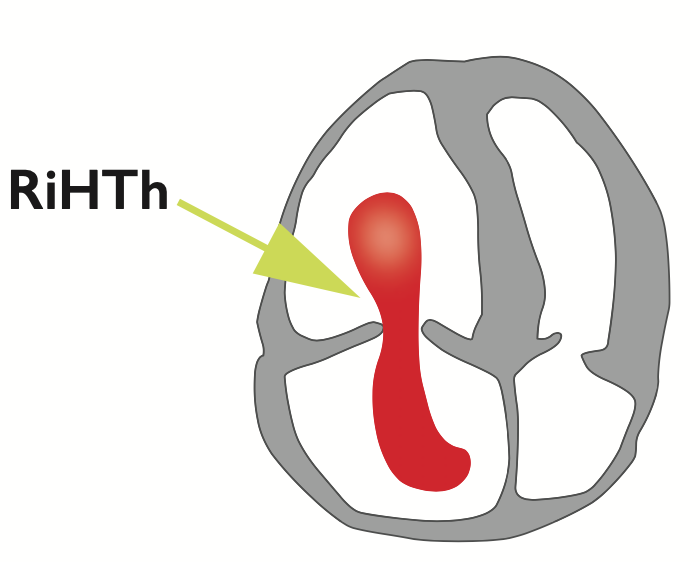
Mobile thrombus in the right heart
Question No. 14
Q: What are the indications for thrombolysis in PE?
Answer No. 14
- High-risk (massive) PE
- Selected cases of intermediate-risk (sub-massive) PE:
- Currently not routinely recommended by ESC guidance
- Some evidence it improves long term outcomes
Question No. 15
Q: What is the role for thrombolysis in sub-massive PE?
Answer No. 15
- Some argue in favour of thrombolysis given improved longer-term outcomes:
- Reduced burden of chronic RV failure or thrombus-related pulmonary hypertension
- Others argue against thrombolysis given:
- Relatively low mortality rates even with standard treatment (heparin)
- Lack of proven mortality benefit (PEITHO trial used composite endpoint of mortality and haemodynamic instability)
- Known potential for serious morbidity/ mortality with thrombolytics (mainly due to intracranial bleeding)
- Increased cost
- European Society of Cardiology guidelines do not currently recommend thrombolysis for intermediate-risk (sub-massive) pulmonary embolism
Question No. 16
Q: What is the evidence for thrombolysis in intermediate-risk (sub-massive) PE?
Answer No. 16
Study
Intervention
Population
Conclusion
- Thrombolysis (tenecteplase 30-50mg & heparin) vs. no thrombolysis (placebo & heparin) in patients with intermediate-risk/sub-massive pulmonary embolism
- 1006 patients across 76 sites in 13 countries
- PE confirmed by V/Q, CT or pulmonary angiogram with RV dysfunction confirmed by echo or CT and raised troponin
- Primary outcome: Death or haemodynamic decompensation (composite endpoint) within 7 days significantly lower in thrombolysis group than placebo group (2.6%5.6%)
- Secondary outcomes:
- No significant difference in mortality (1.2% vs. 1.8%)
- Both major extracranial bleeding (6.3% vs. 1.2%) and haemorrhagic stroke (2% vs 0.2%) significantly higher in thrombolysis group
- Thrombolysis (tenecteplase & heparin) vs. no thrombolysis (heparin alone) in patients with intermediate-risk/sub-massive pulmonary embolism
- 83 patients across 8 sites in the USA
- PE confirmed by V/Q, CT or pulmonary angiogram with RV dysfunction confirmed by echo, troponin or BNP
- Composite primary outcome of death, intubation and major bleeding at 5 days or recurrent PE or impaired functional capacity at 90 days
- Significantly reduced adverse outcomes in thrombolysis group (15% vs. 37% had at least 1 adverse outcome)
- Thrombolysis with half standard dose thrombolysis (tPa & enoxaparin) vs. anticoagulation alone in 'moderate PE'
- 121 patients in single centre in the USA
- 'Moderate PE' defined as haemodynamically stable PE with >70% involvement of thrombus in ≥2 lobar or left or right main pulmonary arteries
- Primary outcome of development of pulmonary hypertension (pulmonary artery systolic pressure ≥ 40mmHg) significantly lower in thrombolysis group than control group(16% vs. 57%)
Question No. 17
Q: What surgical and catheter reperfusion therapies are available and what are their roles?
Answer No. 17
- Should be considered:
- Where there are absolute contraindications to thrombolysis
- Where thrombolytic therapy has failed and the patient is critically ill
- Options include:
Percutaneous Catheter-Directed Thrombolysis / Embolectomy
- Involves insertion of a catheter into the pulmonary arteries via the femoral route
- Different approaches involve one or a combination of:
- Mechanical fragmentation
- Ultrasound fragmentation
- Thrombus aspiration
- In situ reduced-dose thrombolysis
- Overall procedural success rates in small studies have reached 87%
Surgical Embolectomy
- Carried out with cardiopulmonary bypass, with aortic cross-clamping and cardioplegic cardiac arrest
- Involves incision of the two main pulmonary arteries with the removal or suction of fresh clots
- Has favourable outcomes in small studies:
- Similar 30-day mortality to thrombolytic therapy
- Lower risk of stroke or re-intervention
Question No. 18
Q: What are the options for anticoagulation for a patient presenting with pulmonary embolism?
Answer No. 18
Acute Management
Parenteral, weight-adjusted anticoagulation should be used:
- Low-molecular weight heparin (LMWH) SC
- Fondaparinux SC
- Unfractionated heparin (UFH) IV
- Generally second line due to higher bleeding risk and HIT risk
- Preferred agent in the setting of:
- Overt haemodynamic instability or imminent haemodynamic decompensation in whom primary reperfusion treatment will be necessary (short half life and easy reversal)
- Increased risk of bleeding
- Serious renal impairment (creatinine clearance <30 mL/min)
Longer-Term Management
Started when the patient's condition is stable and no invasive procedures are planned
- Non-vitamin K oral anticoagulant (NOAC)
- Warfarin international normalized ratio (INR) is 2.0 to 3.0:
Question No. 19
Q: When should anticoagulation be commenced?
Answer No. 19
- Anticoagulation should be initiated without delay, while diagnostic workup in progress, in patients with:
- Suspected PE with haemodynamic instability
- Suspected PE without haemodynamic instability with a high or intermediate clinical probability
Question No. 20
Q: When should intubation be considered in pulmonary embolism?
Answer No. 20
- Patients at high risk of deterioration during induction of anaesthesia, intubation, and positive-pressure ventilation:
- Effect of drugs on hypotensive patient
- Positive intrathoracic pressure reduces venous return and exacerbates RV dysfunction
- Intubation should be performed only if the patient is unable to tolerate or cope with non-invasive ventilation or high-flow oxygen therapy
Question No. 21
Q: How should right ventricular failure be managed in pulmonary embolism?
Answer No. 21
Fluid Therapy
- Cautious fluid therapy may improve haemodynamic status:
- Small fluid boluses (500ml) have been shown to improve cardiac output
- Aggressive volume expansion should be avoided:
- Potential to over distend the RV and lead to reduced systemic cardiac output
- Not shown to be of benefit in studies and may be harmful
- If signs of elevated CVP, further volume loading should be withheld
Vasopressors & Inotropes
- Noradrenaline considered as first line therapy:
- Increases RV inotropy and systemic blood pressure
- Restores coronary perfusion gradient and improves ventricular interactions
- Dobutamine may be considered useful for patients with PE, a low cardiac index and normal:
- Potential to aggravate ventilation/perfusion mismatch
- Can worsen circulatory failure given vasodilatory effect
Pulmonary Vasodilators
- May be useful in in patients with PE and pulmonary hypertension, though anecdotal evidence only
- Options include inhaled nitric oxide and aerosolised prostacyclin
Mechanical Circulatory Support
- May be useful in the setting of circulatory collapse or cardiac arrest:
- VA-ECMO most frequently used:
- Associated with a high incidence of complications, even when used for short periods
- Effectiveness depends upon centre experience and patient selection